Most people don’t realize that tiny molecular “gatekeepers” called brain transport proteins are the unsung heroes (and sometimes villains) of our nervous system. In a nutshell, these proteins decide what gets in and out of the brain’s most protected zone – the blood‑brain barrier (BBB). If they work well, nutrients, hormones, and even life‑saving medicines slip through smoothly. If they’re broken, the results can be devastating, ranging from subtle metabolic hiccups to severe epileptic encephalopathy.
In the next few minutes, I want to walk you through what these proteins actually do, why they matter to everyday health, and how scientists are turning their quirks into therapeutic opportunities. Think of it as a friendly coffee‑chat where we explore the science, share a couple of real‑world stories, and finish with some practical take‑aways you can use or pass along.
What Are They?
Definition and Major Families
At their core, brain transport proteins are specialized membrane proteins that shuttle ions, metabolites, or larger molecules across cellular barriers. In the brain they fall into a few big families:
| Family | Key Member | Primary Cargo | BBB Role |
|---|---|---|---|
| SLC (Solute Carrier) | SLC13A5, SLC2A3 (GLUT3) | Citrate, glucose | Carrier‑mediated uptake |
| ABC (ATP‑Binding Cassette) | ABCA1, ABCG2 | Lipids, xenobiotics | Efflux & protection |
| DMT (Divalent‑Metal Transporter) | DMT1 | Iron (Fe²⁺) | Iron homeostasis in neurons |
| LAT (L‑type Amino‑Acid Transporter) | LAT1 | Large neutral amino acids | Drug‑carrier gateway |
Each family follows a distinct transport mechanism, but they all share the same mission: keep the brain’s chemistry just right.
Why They Matter
Imagine trying to drive a car across a toll bridge that only lets through vehicles with the right pass. Brain transport proteins are that toll system. They let in glucose for energy, iron for enzyme function, and even therapeutic compounds that could treat Alzheimer’s or epilepsy. When the system malfunctions, the “toll” either blocks vital supplies or lets in harmful substances, leading to disease.
Crossing the BBB
Carrier‑Mediated vs. Receptor‑Mediated Transport
There are two principal ways drugs hitch a ride across the BBB:
- Carrier‑mediated transport (CMT): Uses SLC or LAT proteins that normally ferry nutrients. Scientists attach drug molecules to these nutrients, essentially disguising the drug as a “regular passenger.”
- Receptor‑mediated transcytosis (RMT): Exploits receptors such as the transferrin receptor. A drug is linked to an antibody that binds the receptor, prompting the cell to engulf and shuttle it across.
Both strategies have their pros and cons, but the carrier approach is especially popular for small‑molecule drugs because it’s less likely to trigger immune reactions.
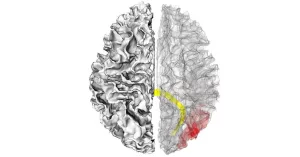
Case Study: 3‑D Modeling of Choline Release
Researchers recently built a 3‑D computer model of a choline‑transport protein to see how it reshapes itself during substrate passage. According to a Frontiers review on DMT1, the protein flips open like a flower, briefly exposing a pocket where choline slides in, then closes to hide it from the extracellular space. This visual evidence helps drug designers predict how to “fit” a therapeutic molecule into the same pocket, increasing the chance it will cross the BBB safely.
When Things Go Wrong
Faulty Transport Protein and Severe Epileptic Encephalopathy
One of the most heartbreaking examples of a broken brain transport protein is the mutation of SLC13A5, the citrate transporter. When this protein can’t move citrate into neurons, the brain’s energy balance goes haywire, triggering a form of early‑onset epilepsy known as severe epileptic encephalopathy. Families often describe the seizures as “lightning fast” and the developmental delays as “impossible to predict.”
If you’re curious about the underlying mechanics, here’s a quick snapshot: citrate normally fuels the tricarboxylic acid (TCA) cycle, the engine that powers neuronal metabolism. Without enough citrate, neurons scramble for alternative fuels, producing toxic by‑products that destabilize electrical signaling.
Impact on Neuron Metabolism
The ripple effect reaches far beyond seizure activity. Neuron metabolism becomes erratic, impairing synaptic plasticity—the foundation of learning and memory. In other words, a single faulty protein can cast a shadow over the entire brain’s ability to adapt and grow.
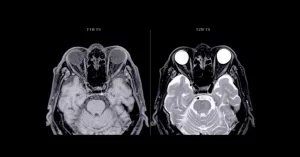
Iron Overload and Neurodegeneration
Another family member, DMT1, is a heavyweight when it comes to iron transport. While iron is essential for making neurotransmitters, too much of it is a neurotoxic nightmare. The 2015 Frontiers review highlighted that DMT1 abundance in brain‑capillary endothelial cells correlates with iron accumulation in Alzheimer’s and Parkinson’s disease brains. Excess iron fuels oxidative stress, which in turn damages neuronal DNA and membranes.
ABC Transporters: Double‑Edged Swords
ABC transporters, like ABCG2, are the brain’s vigilant “security guards.” They kick out harmful xenobiotics, but if they pump out therapeutic drugs too efficiently, treatment fails. A 2024 perspective in Neural Regeneration Research suggests that fine‑tuning these guards could open new doors for neuro‑protective therapies.
Therapeutic Strategies
Trojan‑Horse Drug Design
Imagine smuggling a secret note past a strict bouncer by hiding it inside an allowed item—like a snack. That’s exactly what scientists do with “Trojan‑horse” drugs. By linking a therapeutic agent to a molecule that a transport protein naturally carries (glucose, amino acids, or even a small peptide), the drug sneaks across the BBB under the radar.
Current Pipelines and Clinical Trials
- LAT1‑linked prodrugs: In early‑phase trials for glioblastoma, these compounds show up to 4‑fold higher brain concentrations than their unmodified counterparts.
- Glucose‑conjugated antioxidants: A Phase II study reported improved cognitive scores in mild Alzheimer’s patients, likely because the drugs rode the GLUT3 pathway into neurons.
Gene‑Therapy and CRISPR Corrections
For conditions rooted in a single genetic error—like SLC13A5 epilepsy—gene‑editing offers a tantalizing hope. Researchers are testing AAV‑delivered CRISPR systems that replace the faulty gene copy in mouse models, restoring normal citrate transport and dramatically reducing seizure frequency.
Balancing Risks and Benefits
Every intervention carries a trade‑off. Over‑enhancing a transporter could flood the brain with unwanted substances; under‑dosing may leave the disease untouched. That’s why clinicians monitor plasma drug levels, neuroimaging biomarkers, and, importantly, patient‑reported outcomes throughout treatment.
Balancing Benefits and Risks
Key Takeaways
- Brain transport proteins are essential for nutrient supply, waste removal, and drug delivery.
- Mutations such as those in SLC13A5 or dysregulation of DMT1 can trigger severe neurological disorders.
- Modern therapies are learning to “hijack” these proteins safely, turning a vulnerability into a strength.
- Because the BBB is a protective wall, any manipulation must be carefully calibrated to avoid collateral damage.
Practical Checklist for Clinicians & Patients
- Screen for known transport‑protein gene variants (SLC13A5, DMT1, ABC families) when unexplained seizures or neurodegeneration appear.
- Consider carrier‑mediated drug formulations if standard therapies fail to reach therapeutic brain concentrations.
- Monitor iron levels and oxidative‑stress markers in patients with chronic neurodegenerative disease.
- Stay informed about emerging gene‑editing trials—many are recruiting and may offer a lifeline for rare epilepsies.
Conclusion
Brain transport proteins sit at the crossroads of physiology and pathology. When they function properly, they keep our thoughts, movements, and memories humming along like a well‑tuned orchestra. When they falter, the consequences can be severe—but they also give science a clear target to aim at. By understanding these proteins, we empower ourselves to ask the right questions, support smarter drug design, and maybe one day turn even the most devastating epileptic encephalopathies into manageable conditions.
If you’ve ever wondered why a medication works for some people but not for others, or why certain genetic disorders affect the brain so profoundly, the answer may lie in these tiny yet mighty gatekeepers. Keep exploring, stay curious, and remember: the brain’s mysteries are complex, but with the right knowledge, they become a little less intimidating.




















Leave a Reply
You must be logged in to post a comment.