Alright, let’s cut to the chase. If you’re here, you’re probably staring down a diagnosis of SLC13A5 epilepsy—or you’re researching for someone who is. Either way, this stuff can feel like looking inside your brain and thinking, “Whoa, what’s broken?” I get it. Your brain’s like a car, and SLC13A5? It’s the gas tank getting empty in real time. Citrate, which fuels your neurons? Without it, your brain throws a wild, noisy party called seizures. And it’s not just one patient filing this complaint—it’s dozens, and maybe hundreds, across the world. Let’s dive in together.
What’s the Big Deal?
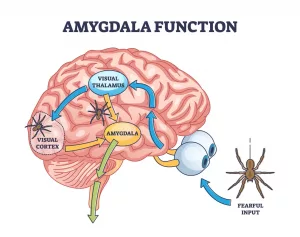
SLC13A5 epilepsy. Sounds fancy, right? But here’s the lowdown: your brain runs on energy. Neurons? They absolutely need a compound called citrate, and when a protein called SLC13A5 isn’t doing its job… you guessed it… seizures, developmental delays, and a host of other issues. And this isn’t some background noise of a disease—it’s a full-on neurological firefight. We’re talking unrelenting, early seizures and families watching their babies fight for normalcy.
So why is this transport protein such a big deal? Imagine this: your brain starving for fuel while you eat, sleep, and play like normal. SLC13A5 is supposed to shuttle citrate into neurons so they can metabolize, grow, and communicate like they should. But if it’s faulty or missing—well, that’s severe epileptic encephalopathy 101.
Brain Protein, Big Problems
Here’s the quiet truth: SLC13A5 isn’t just any brain transport protein. It’s THE gatekeeper for citrate, a metabolic building block. When it’s not working because of autosomal recessive mutations? Neuronal metabolism takes a nosedive. Got all that? Trust me—it’s less sci-fi than it sounds.
We’re not making this up. Preclinical research in PMC9498415 shows that people with faulty SLC13A5 experience energy-starved neurons. No citrate = no brain development. No development = seizures… and much, much more. You’ll hear more about this soon.
Treatment: Where Are We Going?
Right now, “treatment” mostly means trying to stem the bleeding—meds to stop seizures and diets to stabilize the brain’s energy supply. But everyone’s got the same question: “Is this really all we’ve got?” Not to layer on the anxiety, but there’s a reason parents and caregivers are keeping gene therapy as a hope-filled keyword in their search box for SLC13A5 epilepsy.
Medications: Clunky, Not Curative
Anti-seizure meds (ASMs) are typically the go-to strategy. You’ve likely seen lists like, “Top three meds,” “Best combo therapies,” etc. Real talk—some combinations do work… but often only partially. PMC9498415 drops the heavy truth: current medications don’t fix developmental delays, intellectual disability, or tooth development issues.
And training wheels like Ketogenic Diet occasionally step in. Will they fix flaws in brain transport protein pathways? Not quite. But they can reduce seizures—imagine throwing water on one spark in a firestorm. Not perfect… but something, right?
Real-World Challenges
| Treatment | Addresses Seizures? | Supports Development? |
|---|---|---|
| ASMs (Anti-Seizure Meds) | Some control | Almost none |
| Ketogenic Diet | Moderate benefit | Minimal data |
| Gene Therapy (potential) | Promising experimental control | Yes—could may change developmental outcomes |
Each patient’s situation is different. Some bend under the pressure trying multiple ASMs with mixed results. Others try alternative nutrition while silently fearing the days ahead. Understandable, right? “Partial” just doesn’t cut it for families figuring out what happens next.
Gene Therapy: The Big “What If”
Now here’s where things get intense. AAV9-based gene replacement therapy—basically inserting functional SLC13A5 genes where the bad ones lived—has stirred excitement in the research community for SLC13A5 epilepsy.
TSHA-105: Where’s It At?
Back in 2022, there were whispers of trials kicking off soon for TSHA-105. Fast forward… and as of 2023, things got quiet. According to a SEC.gov filing from that same year, Taysha Gene Therapies hasn’t stopped the work—it’s just… waiting.
“None of us wanted to delay. But science? It has its own timeline.” — TESS Research Foundation, 2024
The foundational idea? If we can replace the gene and restore that SLC13A5 epilepsy link to normal citrate transport, maybe—just maybe—we can rescue those neurons. Trials may assess outcomes like seizure reduction and developmental improvements. That’s new. Most treatments barely touch the latter. Now family rumors for FDA go-rounds in 2025 remain bragged on, but nothing’s confirmed.
What Could Go Right?
Gene therapy’s like throwing a lifeline to people on a sinking boat. According to publications in Bioengineer.org: restoring SLC13A5’s faulty transport protein function may literally normalize synaptic transmission. It’d stop the firing. Kickstart metabolism. Slow neurodegeneration? Possibly. You don’t just dabble with genes for fun—you do it when there’s no other Hope Bus leaving.
What Could Go Wrong?
Okay, but no fairytale comes without a “what if.” AAV9 is generally safe, right? But let’s not kid ourselves—if this is the first real big test for SLC13A5, what dose_adaptation, potential vector immunity, or even treatment success, is a gamble.
A 2023 Springer paper candidly noted the same risks in other gene therapies for epilepsy. But here’s the gut punch: with peer-reviewed preclinical research already submitted in PMC11292725, can we afford not to try?
Science On The Sideline
Wait, let’s backslap for a sec. How does a faulty transport protein in the brain actually steeper seizures and development hiccups?
Because citrate is neuro-fuel. Post-slc13a5 deficiency? That fuel train gets derailed. Neurons can’t metabolize right, and BAM—synapses start misfiring like champagne corks after a big cork-popping science party. No balance. Too much excitement. Seizures happen.
Seizures, But Also the ‘Invisible’ Symptoms
Slc13a5 isn’t just about Big Seizure Drama. Though neonatal seizures might be your first indicator, researchers in a Medical News Today article highlight that symptoms include non-epileptic challenges, like cognitive delays and tooth enamel issues—part of that under-discussed parent-to-parent support call.
It’s extra messy because the transporter issue isn’t picky—it’s affecting brain and body metabolism. So while a child sleeps and eats, they’re still fighting a ton of neural logistics. You’d never see it from the outside. That’s part of what makes SLC13A5 epilepsy no joke—invisible, but jaw-droppingly severe.
The Fine Line: Hope Without Fake Promises
Look. If you’re walking into this condition with guarded hope, good for you. Evidence for this clinical approach isn’t sitting on a shelf. But RareDiseases.org can vouch—anything targeting the underlying genetic flaw ranks higher than tampering with symptoms long-term. There’s current work. It’s real. It’s slow.
Here’s the point: don’t give your trust to “cure clickbait.” Rogue clinics, pseudo-science bros, and miracle-promising newsletters? All off the table. We want reputable advances, not sketchy crypto-drug-dealers on a clinical premise.
Gene Therapy Snags
All right, here’s the deeply human side of this: in a 2023 patient survey, families were—understandably—impatient. Trials paused. But TESS Research Foundation keeps agencies afloat. Offers brilliant library of info. Keeps scientific communities fused to families.
Because human studies haven’t kicked off, we’re stuck… again. And again. What’s worse, patient privacy bars us from using identifying stories—understandable, given how small this population is. But here’s hoping AAV9-based treatments go beyond the current allowed frameworks and elevate our narrative.
What’s the Status of TSHA-105 Today?
If you’re looking to join a trial yesterday… I have bleak news. There’s no date. PMC11292725 has bits on methodology empowerment—but we’ve got no timeline for clinical kicks yet. And the question we’ve been asking since Day One? Can we tolerate delays in a disorder that hits newborns? The heartbreak here is deep.
What Now For Families?
If you’ve been asking, “Should I go primal with turmeric enemas, or just wait for frontliners?” I side-eye the first. Please—stick with medical professionals. Targeting brain transport protein glitches with science? That’s the way. Here’s some solid steps to take.
Find a Genetic Specialist You Can Lean On
Are you seeing if there’s a mutation in SCN1A or STXBP1 and wondering, “Is SLC13A5 the real thief behind the curtain?” A certified clinical geneticist, hooked up to the Epilepsy Foundation’s network, can dig deeper than solo tests.
How Patient Groups Help
TESS Research Foundation? That’s your home. They’re keeping flame lit for disorders like this. Patient registries? They’ve got ‘em. Mapping genetic epilepsy territories? Yep, they’re in the front seat. So take your questions to these folks. They’re doing the real, methodical hustle—not selling dreams.
Keep Your Options Open
Treatment file: favorites include early seizure monitoring, nutrition support, and preclinical study entry. If you’re physicians see trends in neuron metabolism for SLC13A5 patients, it might effect other lines of treatment. And—bonus—it keeps you in the loop for future therapeutic arrivals.
Why It Helps to Finally Know
Understanding SLC13A5 gives families an anchor. You’ve got something to fight, adapt, and take control over. Preclinical studies, TESS, even Facebook epilepsy groups (yes. Real. Groups exist.) create camaraderie.
When we finally unpack how these mutations cause such brain transport meltdowns, somewhere, a cold treatment approach will thaw. Every lost month erodes our patience, but knowing the answer is this close keeps us searching. Every scientific peer-review drops us one shelf closer to a pediatric solution.
More Than Number of Seizures
The human bit of all this? It’s not just about how many attacks happened this week—it’s about how we live with this challenge.
I once talked to a parent whose son has SLC13A5. She summed it up this way: “We’re trying not just to stop the shaking—but to finally get his mind on track. The meds calmed some spasms. But the delays… they linger like a penumbra.”
That’s the landscape. Seizures are urgent. Development is audacious.
Your Path Forward
So yeah, feeling stuck without a birthdate for intervention-grade gene therapy for SLC13A5 epilepsy is a big rough draft of now. But what saves you? Layers of individualized care, strong family circles, and gene replacement knowledge building on preclinical momentum.
Let’s be real. You can’t ABBA’s “Take a Chance on Me” your way through this. But you can engage the right community. Talk to trusted neurologists. Save trial timelines to your Google Calendar. Monitors for TSHA-105 drops? Of course.
This stuff isn’t fringe. It’s a real problem. For science. For families. And the answer’s in the lab—isn’t that the kind of hope worth holding onto?
Stay Connected
If things push forward, methods get sharper, and patients finally rally—TESS Research will likely be the first to tell you. Their foundations track treatment, advocate for pipeline changes, and stabilize another run of research. If you’re not joined to their mailing lists or private forums—please do it now. It’s not noisy. It’s your best shot at real treatment radar.
Chasing Science But Grounded
Think of this like a family road trip. Your destination? Functional neurons, less seizures, less neurodevelopmental setbacks. The GPS? Science. But sometimes it reroutes. Sometimes it stalls. Don’t look for shortcut exits. Stay with guides and data.
All I’m saying is this: fuel yourself with hope, but don’t basement-panic. Epilepsy & metabolism science is still catching up—and metaphorically… neuroscience is now on the next research leg. Let’s hike this trail. Together, maybe our “next step” is a breakthrough.
What You Can Do Today
| Tip | Action |
|---|---|
| Verify Genetic Cause | Confer with a genetic counselor or hospital lab for accurate SCN1A/STXBP1/SLC13A5 ruling |
| Stay Informed | Follow PMC and_registry studies for progress updates |
| Explore Patient Resources | Visit TESS’ site, which holds transparent guides |
So What’s the Takeaway?
There’s no workaround rail for this condition—and yet, there’s a spark. Preclinical work in Brain Journal: PMC11292725 suggests that SLC13A5 gene expression correction may step into the clinic someday soon. Treatments like TSHA-105? They’re still holding near the starting line.
ASMs help—but they don’t “solve” it. Ketogenic diet helps mostly season the plateau. But a breakthrough in brain transport protein replacement? That’s the kind of game-changing content we study up now, hold while we wait, and keep sharing. For families researching SLC13A5 epilepsy? You’re already smarter than the internet. Now, let’s keep fighting forward—even if it’s challenging until that treatment date drops. First science. Then solutions. Then, growth.
You’re Not Alone
While some folks wrap their lives around eating kale or crypto bots, we’re here to heal a gene. Faulty transport? Metabolic nerves out of whack? Join us in prioritizing clarity over chaos.
If this post helped light up something fuzzy about SLC13A5 epilepsy—for you or someone you love—we’re glad. But more importantly, you’re heard. Keep staying curious, keep advocating, and when you want a virtual hug on this front… well, we’re here, too.
What does the transport look like to you? Do tell. Have a question we skipped? Comment section’s open. Because if we’re gonna understand this—or any—children’s epilepsy deeply, we’ve got to keep the science shared, and the tone warm. Because humans, not machines, really get this.
Questions For You
Do you feel unprepared when managing symptoms of SLC13A5 at home? Are genetic conferences too clinical-speak-choked to follow?
If you’re a caregiver with long hairs still sticking out in the wind… what’s the smallest win? Or the biggest confusion? Drop a note. Let’s keep this moving forward… together.





















Leave a Reply
You must be logged in to post a comment.