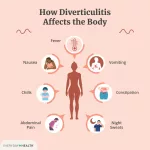
Vagus nerve stimulation (VNS) is a medical therapy that sends tiny electrical pulses to the vagus nerve, a key player in the body’s “rest‑and‑digest” system. It’s most famous for helping people whose seizures or depression haven’t responded to medication, but it’s also being explored for migraines, stroke recovery, and even autoimmune disorders.
If you’ve heard doctors mention a “vagus nerve device” or you’re curious whether an implantable nerve stimulator might be right for you, this article is your friendly guide. I’ll walk you through how VNS works, who might benefit, the real‑world pros and cons, and what life looks like after the surgery— all in a conversational tone, like we’re having coffee and chatting about health choices.
How VNS Works
Vagus anatomy in a nutshell
The vagus nerve is the longest cranial nerve, winding from the brainstem down through the neck, chest, and into the abdomen. It’s the main conduit of the parasympathetic nervous system, slowing heart rate, aiding digestion, and even influencing mood. Because it carries about 80 % sensory fibers, stimulating it can send signals straight to the brainstem and, from there, to regions that regulate seizures and emotional states.
What the device actually does
Think of the vagus nerve stimulator as a tiny pacemaker for your nerve. The pulse generator (the “battery” about the size of a silver dollar) sits under the skin in the upper chest. A thin lead wire runs up the side of your neck and wraps around the left vagus nerve—surgeons usually avoid the right side because it’s closer to the heart and can affect heart rhythm.
When activated, the device emits short bursts of electricity. Typical settings might look like this:
| Parameter | Typical Value |
|---|---|
| Frequency | 20 Hz (pulses per second) |
| Pulse width | 250 µs (microseconds) |
| On‑time / Off‑time | 30 s on, 5 min off |
| Current strength | 0.25–3.5 mA, titrated gradually |
These settings are customized by your physician using a handheld programming wand. The goal is to modulate the brain’s electrical environment just enough to reduce seizures or lift mood without causing uncomfortable side effects.
Why left‑side only?
The left vagus nerve has fewer direct connections to the sinoatrial node, the heart’s natural pacemaker. Stimulating the right side could unintentionally speed up your heart rate or cause arrhythmias. That’s why most VNS therapy protocols stick to the left side—a safety detail you’ll hear repeated in the OR briefing.
Who Benefits
FDA‑approved uses
According to the Mayo Clinic, the U.S. Food and Drug Administration has green‑lit VNS for:
- Focal epilepsy in patients age 4 years and older who haven’t found seizure control with at least two appropriate anti‑seizure medicines.
- Treatment‑resistant depression (TRD) in adults who have failed four or more medications, electroconvulsive therapy, or both.
- Post‑stroke upper‑limb rehabilitation (approved under a separate indication for improving motor recovery).
- Cluster headaches and migraines (non‑invasive devices, see later).
Exploratory and off‑label areas
Researchers are peeking into many more possibilities—rheumatoid arthritis, Alzheimer’s disease, obesity, and even chronic pain. A recent review in Neurophysiotherapy highlighted promising early‑phase trials for inflammatory bowel disease and bipolar disorder (NCBI).
Is VNS right for you?
Ask yourself these quick questions (you can jot down notes while you read):
- Have you tried at least two appropriate medications for epilepsy or depression without sufficient relief?
- Do you have a clear diagnosis from a neurologist or psychiatrist who understands VNS?
- Are you comfortable with a minor surgery and periodic device checks?
- Do the potential benefits—fewer seizures, mood lift, better motor function—outweigh the known side effects for you?
If the answer is “yes” to most, you might be a solid candidate. Always bring these points to your specialist’s office; they’ll help you weigh the risks and rewards.
Pros and Cons
Proven benefits
Clinical data are encouraging. About 30 % of patients with refractory epilepsy see a ≥50 % reduction in seizure frequency after a year of VNS (Cleveland Clinic). For depression, roughly 20‑30 % achieve a meaningful response, and another 10‑15 % attain remission after extended therapy.
Common side effects
The most frequent complaints are mild and often improve with programming tweaks:
- Hoarseness or a “talky” voice during stimulation.
- Throat tickle or cough.
- Shortness of breath when the device is on (usually at higher current).
Most people adapt within weeks. Your physician can lower the intensity or adjust the on/off cycle if symptoms linger.
Surgical and long‑term risks
Because VNS involves a small operation, you inherit the usual surgical risks: infection, bleeding, and rare nerve injury. Battery life is finite; the pulse generator typically lasts 5‑10 years, after which a replacement surgery is needed (still a short outpatient procedure). A study from the Mayo Clinic reported infection rates below 2 % and no permanent nerve damage in the majority of cases.
Balancing the scales
Think of VNS like a bridge: it’s built to cross a difficult gap (uncontrolled seizures or stubborn depression). The bridge costs money, time, and a bit of maintenance, but once you’re on the other side, daily life can feel dramatically lighter. My own friend, a teacher named Maya, described it as “getting a tiny, invisible coach whispering encouragement to my brain every few minutes.” That personal touch—knowing there’s a device working behind the scenes—often turns anxiety about the unknown into cautious optimism.
Device Types
Implantable (iVNS)
The classic VNS system is an implantable nerve stimulator placed under the skin of the left chest. It’s reliable, has the longest track record, and can be programmed to very precise settings. The downside? It requires surgery and a battery that will eventually need swapping.
Non‑invasive (tVNS / nVNS)
For headaches or people who shy away from surgery, there are transcutaneous options that clip onto the ear or sit on the neck surface. The FDA has cleared a device for acute treatment of cluster headaches and migraines—no incision, no battery replacement, just a small handheld unit that you press against the skin.
Side‑by‑side comparison
| Feature | Implantable (iVNS) | Non‑invasive (tVNS/nVNS) |
|---|---|---|
| Invasiveness | Surgical implantation | Surface application only |
| FDA‑approved uses | Epilepsy, TRD, stroke rehab | Cluster headache, migraine |
| Battery life | 5‑10 years (replaceable) | Rechargeable, lasts weeks per charge |
| Cost (US) | $30K‑$45K (incl. surgery) | $2K‑$4K (device only) |
| Programming | Clinic‑controlled via wand | User‑controlled via app or button |
The Procedure
Before you go under the knife
Doctors will run a series of checks: blood work, a brief cardiac exam, and a conversation about your medication history. You may get a pre‑op MRI to map the anatomy, though the final “go” signal often comes after a multidisciplinary team reviews your case.
Step‑by‑step surgery
- Incision 1 – the neck: A 2‑cm cut on the left side exposes the vagus nerve.
- Incision 2 – the chest: A second incision in the upper left chest creates a pocket for the pulse generator.
- Lead placement: The surgeon gently wraps the coil electrodes around the nerve and threads the insulated wire down to the chest pocket.
- Generator implantation: The battery‑like device is placed under the pectoralis fascia, then sewn in place.
- Testing: With the wound still open, the team turns the device on at a low setting for 30–90 seconds to confirm proper nerve capture.
The whole operation usually takes 45‑90 minutes. Most patients go home the same day, though some doctors prefer an overnight observation for comfort.
Recovery and first activation
After surgery you’ll get wound care instructions and a short course of antibiotics to lower infection risk. Two to four weeks later, you return to the clinic for the first “turn‑on.” Using a specialized wand, the neurologist programs the device to a gentle baseline; then, over several weeks, the settings are slowly increased based on how you feel and any side effects that arise.
Living With VNS
Daily life tweaks
Most people resume normal activities within a week. There are a few practical points to keep in mind:
- MRI safety: Modern devices are “MRI‑conditional,” meaning you can have scans after the device is set to a special mode (ask your radiology department).
- Metal detectors: You’ll pass through, but the metal coil may set off a beep. A quick “I have a medical device” note usually clears it.
- Exercise: Light cardio, yoga, and strength training are all fine; just avoid heavy contact sports that could damage the chest pocket.
Magnet for on‑the‑spot help
Many pulse generators come with a handheld magnet. Swiping it over the device temporarily turns the stimulation off (or on, depending on the model) for about 30 seconds—useful if you experience a sudden cough or voice change and need a quick break.
Battery life and costs
The generator’s battery is a sealed, non‑rechargeable cell that slowly depletes. When the device signals low power (a subtle vibration or a clinic alert), you’ll schedule a replacement surgery. Insurance typically covers the majority of the cost, especially for FDA‑approved indications, but out‑of‑pocket expenses can range from $5,000‑$10,000 for the battery swap.
Tracking progress
Doctors love numbers, so they’ll ask you to keep a seizure diary or depression rating scale (like the PHQ‑9). Over months, you’ll see trends—perhaps fewer seizures, a brighter mood, or improved hand strength after a stroke. Celebrate each small win; they’re the proof that the little pulses are doing big work.
Evidence & Guidelines
Landmark trials
The first VNS trial for epilepsy in 1997 enrolled over 200 participants and demonstrated a 24 % reduction in seizure frequency compared with control (Wikipedia). The 2005 depression trial showed that after one year, 31 % of patients had at least a 50 % drop in Hamilton Rating Scale scores.
Recent systematic reviews
A 2024 meta‑analysis in Neurophysiotherapy pooled data from 27 studies and confirmed that VNS reduces seizure frequency by an average of 35 % and improves quality of life metrics across age groups. The same review highlighted a modest but statistically significant improvement in depressive symptoms, especially when VNS is combined with ongoing psychotherapy.
Professional guidelines
According to the American Academy of Neurology (AAN) and the FDA, VNS should be considered after at least two appropriately chosen anti‑seizure medications have failed, and patients should have realistic expectations about gradual symptom improvement (FDA).
Future Directions
Closed‑loop systems
Next‑generation VNS devices are learning to “listen” as well as “talk.” Sensors embedded in the lead can detect abnormal brain activity (like an impending seizure) and automatically increase stimulation—a concept called responsive or closed‑loop VNS. Early trials show faster seizure abort rates and reduced overall stimulation time.
Broadening the therapeutic horizon
Researchers are testing VNS for inflammatory bowel disease, Parkinson’s disease tremor control, and even chronic pain syndromes. The mechanism appears linked to the vagus nerve’s role in the cholinergic anti‑inflammatory pathway—stimulating the nerve can dampen systemic inflammation, a promising angle for autoimmune conditions.
Consumer‑grade wearables
By 2025, a handful of FDA‑cleared wearable VNS devices have entered the market for migraine relief. They’re not a replacement for the implantable system but illustrate how the technology is moving into everyday life. Expect more sleek designs, smartphone‑linked apps, and personalized dosing algorithms in the near future.
Wrapping Up
Vagus nerve stimulation is a fascinating blend of neurology, engineering, and personal empowerment. It offers a lifeline for those whose seizures, depression, or post‑stroke challenges haven’t yielded to medication alone. Like any medical decision, it carries surgical risks, maintenance duties, and a financial component, but for many the payoff—fewer seizures, steadier mood, regained independence—is worth the journey.
If you think VNS might be a good fit, start by talking with a neurologist or psychiatrist who specializes in the therapy. Bring a list of questions, review the pros and cons, and consider how the device could change your daily routine. And remember, you’re not alone; thousands of patients already walk the path you’re contemplating, and many are eager to share their stories.
What’s your experience with VNS, or what worries you most about it? Drop a comment below, share this article with a friend who’s researching options, or reach out to a support group. Knowledge, empathy, and community are the best companions on any health journey.





















Leave a Reply
You must be logged in to post a comment.