Hey there, friend. If you’re scrolling through medical articles feeling a little overwhelmed by all the jargon, you’re not alone. Getting a needle in your arm can feel like a big step—especially when you’re trying to figure out if you have lupus or how well your treatment is working. Below is a straight‑to‑the‑point, warm‑hearted guide that explains exactly what each test does, why it matters, and how you can team up with your doctor to keep the disease in check. Let’s dive in together.
Why Blood Tests Matter
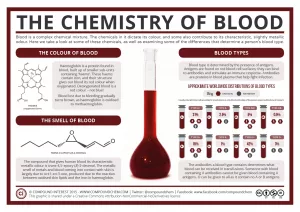
Think of lupus as a sneaky shape‑shifter. Its symptoms can hide behind fatigue, joint aches, or a rash that looks like anything else. Blood work helps us catch the invisible clues that the body is sending. While a doctor can’t diagnose lupus by looking at you alone, the right lupus diagnostic test adds a solid piece to the puzzle.
Benefits of the lab work include:
- Confirming whether an immune system is acting up.
- Identifying which organs might be under attack.
- Tracking how well medication is calming the fire.
- Spotting potential side‑effects before they become a problem.
At the same time, it’s essential to remember that no single test can tell the whole story. That balance of benefits and limits is why we always talk about both the good and the risk of relying on lab numbers.
Core Diagnostic Tests
When a rheumatologist suspects lupus, there’s a standard set of blood work they’ll usually order. Below is a quick reference table that shows what each test looks for, what a typical lupus pattern is, and when it’s most likely to be ordered.
| Test | What It Measures | Typical Lupus Pattern | When It’s Ordered |
|---|---|---|---|
| Complete Blood Count (CBC) | Red cells, white cells, platelets | Low RBC, low WBC, low platelets | First visit – baseline |
| Antinuclear Antibody (ANA) | Auto‑antibodies that target cell nuclei | Positive in ~97 % of patients | Screening “first‑stop” test |
| Anti‑double‑stranded DNA (anti‑dsDNA) | Auto‑antibodies against DNA | Positive in ~50 % of patients; levels rise with flares | Confirmatory, disease‑activity monitoring |
| Anti‑Smith (anti‑Sm) & Anti‑RNP | Specific auto‑antibodies | High specificity for lupus | When ANA is positive but unclear |
| Complement C3 & C4 | Proteins that help the immune system | Low levels indicate active inflammation | Monitoring disease activity |
| Erythrocyte Sedimentation Rate (ESR) / C‑reactive Protein (CRP) | General inflammation markers | Often elevated during flares | Baseline and periodic checks |
These “core” tests are recommended by the Lupus Foundation of America and are echoed in the Mayo Clinic’s diagnostic pathway.
Antibody Test Panel
Beyond the ANA, there’s a whole family of auto‑antibodies that can help refine the diagnosis and sometimes predict which organs might get involved. Here’s a quick rundown of the most common ones.
- Anti‑Ro/SSA & Anti‑La/SSB – Often show up in cutaneous (skin) lupus and can be linked to photosensitivity.
- Antiphospholipid antibodies (aPL) – About half of lupus patients carry these; they raise the risk of blood clots. Johns Hopkins Lupus Center explains their clinical impact.
- Anti‑RNP – May suggest an overlap with mixed connective‑tissue disease.
- Anti‑Sm – Highly specific for lupus, though seen in only ~30 % of patients.
When you get a “lupus antibody test” panel, the lab will usually report which of these antibodies are present and at what titer (strength). The higher the titer, the more likely it is to be clinically relevant—but always interpret it with your doctor’s help.
Monitoring With Labs
Diagnosing lupus is just the opening act; the real marathon begins with ongoing monitoring. Regular lab work tells you whether the disease is calm, flaring, or responding to medication.
Below is a sample 12‑month monitoring schedule that many rheumatologists recommend. Adjustments are common—talk with your provider about what works for you.
| Month | Tests to Repeat | Why |
|---|---|---|
| 0 (diagnosis) | Full panel (CBC, ANA, anti‑dsDNA, complement, ESR/CRP) | Establish baseline |
| 3 | CBC, complement, anti‑dsDNA (if positive) | Check early treatment response |
| 6 | All baseline tests + liver/kidney panels if on immunosuppressants | Monitor organ health & drug toxicity |
| 9 | Complement, ESR/CRP | Detect subtle inflammation |
| 12 | Full panel again | Annual review & adjust meds if needed |
Emerging research, like the LuGENE blood test discussed in Healthline, aims to predict flares before they happen. While promising, it isn’t standard care yet, so stick with the established schedule until your doctor says otherwise.
Reading Your Results
Seeing numbers on a lab report can feel like deciphering a secret code. Here are a few “red flags” that typically prompt a change in treatment:
- Rising anti‑dsDNA or falling complement (C3/C4) – Often signals an upcoming flare.
- New anemia or thrombocytopenia on CBC – May indicate bone‑marrow involvement or medication side‑effects.
- Elevated ESR or CRP – General inflammation, sometimes from infection, so your doctor will check the context.
- Positive antiphospholipid antibodies – Triggers consideration of anticoagulation if clot risk is high.
It’s crucial to remember that a positive ANA alone does not equal lupus. Many healthy folks have a low‑titer ANA. That’s why the big picture—symptoms, physical exam, imaging, and labs—matters more than any single number.
Limits and Risks
Even the best lab tests have blind spots.
- False positives – Certain infections, medications, or even a cold can temporarily raise ANA.
- False negatives – About half of lupus patients never develop anti‑dsDNA antibodies, so a negative result doesn’t rule it out.
- Psychological weight – It’s normal to feel uneasy when results are ambiguous. If you’re nervous, bring a friend to the appointment or write down questions ahead of time.
- Practical concerns – Insurance coverage can vary, and repeated draws may feel inconvenient. Knowing the recommended schedule (see table above) helps you plan and avoid unnecessary repeats.
When you suspect an error, it’s perfectly okay to ask for a repeat test at the same or a different lab. Many clinicians appreciate a proactive patient.
Practical Patient Tips
Here’s a quick checklist to make each lab visit smoother and more informative:
- Preparation: Most lupus labs don’t require fasting, but keep a list of any meds you take (especially steroids or immunosuppressants) because they can affect results.
- Bring a symptom diary: Note joint pain, rashes, fatigue, or new meds from the past two weeks. Your doctor can correlate diary entries with lab changes.
- Ask before you leave: “What does a low C3 mean for me right now?” or “If my anti‑dsDNA goes up, what will we do?”
- Save the report: Store a digital copy in a folder labeled “Lupus Lab Work.” It’s handy when you switch doctors or need a second opinion.
- Know the lingo: “Titer” is the strength of an antibody; “borderline” means it’s close to the cut‑off and may need retesting.
Think of yourself as the captain of a ship. The labs are the weather reports; they help you steer, but you still decide the course with your medical crew.
Trusted Sources & Experts
Good information comes from reputable places. When you read about lupus, look for content that cites:
- The Lupus Foundation of America – a patient‑focused organization that translates research into plain language.
- Mayo Clinic’s rheumatology pages – they break down each test and its clinical relevance.
- Peer‑reviewed studies in journals like Arthritis & Rheumatology (2023) that evaluate the sensitivity and specificity of anti‑dsDNA and complement levels.
- The Johns Hopkins Lupus Center – a leading academic hub for lupus testing protocols.
Whenever you feel uncertain, ask your doctor, “Can you point me to a reliable source for more detail on this test?” A good clinician will welcome an informed patient.
Conclusion
Lupus blood tests are powerful tools that, when paired with a careful review of symptoms and physical findings, give doctors a clearer picture of what’s happening inside your body. No single test can answer every question, but together they let us diagnose earlier, monitor disease activity, and adjust treatment before damage occurs.
Remember, you’re not alone in navigating the lab maze. Keep a symptom diary, ask the right questions, and stay curious about the numbers you see. With the right partnership between you and your healthcare team, those blood draws become less of a mystery and more of a checkpoint on the road to better health.
If you have experiences with lupus lab work—good or confusing—share them in the comments below. Your story might be the exact piece of reassurance another reader needs. And if you’re ready to take the next step, consider downloading our free “Lupus Lab‑Work Cheat Sheet” to bring to every appointment.





















Leave a Reply
You must be logged in to post a comment.