Alright, let’s cut to the chase. Lupus cystitis is a rare bladder inflammation that shows up in people who already have systemic lupus erythematosus (SLE). It often masquerades as a stubborn urinary‑tract infection, a stomach upset, or just “that annoying urge to pee all the time.” If you’ve ever felt seen‑by‑the‑doctors‑and‑still left with more questions than answers, you’re in the right place. In the next few minutes we’ll demystify what lupus cystitis really is, why it happens, how you can spot it, and what you can actually do about it – all in a friendly, down‑to‑earth voice that feels like chatting with a buddy over coffee.
Grab a cup, get comfy, and let’s walk through the whole story together. By the end you’ll know the red‑flags, the treatment options, and practical tips for daily life – so you can feel confident and in control, no matter what your doctor says next.
What Is Lupus Cystitis?
Imagine your bladder is a soft balloon that’s suddenly surrounded by a swarm of tiny, angry immune cells. That’s essentially what lupus cystitis does. In people with SLE, the immune system goes haywire and attacks its own tissues, including the delicate lining of the bladder. The result is swelling, pain, and sometimes a thickened bladder wall that can’t hold normal volumes of urine.
Even though the condition is “rare” – reported in roughly 0.01 % to 2 % of SLE patients – it’s far from insignificant. A small study found that up to 92 % of reported cases occur in women, usually between their 20s and 40s, and many of them experience serious complications if the disease isn’t caught early. According to a narrative review, the underlying culprit is thought to be small‑vessel vasculitis – that’s a fancy way of saying the blood vessels feeding the bladder become inflamed and leaky.
Seeing this through a personal lens, I remember a friend, Maya, who was diagnosed with lupus in her early thirties. She started having “just a little more bathroom trips” and dismissed it as stress. Months later, the urgency turned into pain, and an ultrasound finally revealed a thick bladder wall. That was her “aha” moment: what felt like a minor nuisance was actually lupus cystitis.
Lupus Cystitis Causes
There’s no single villain here, but a handful of usual suspects:
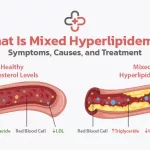
- Autoimmune vasculitis: The immune system creates immune complexes that deposit in the bladder’s micro‑vasculature, causing inflammation. This is the most widely accepted mechanism.
- Anti‑SSA antibodies: Studies from East Asia show a surprisingly high rate of anti‑SSA positivity among lupus cystitis patients. One Chinese cohort even linked these antibodies to more severe bladder wall thickening research.
- Drug‑induced irritation: Some lupus patients receive cyclophosphamide, a chemotherapy‑type drug that can itself cause hemorrhagic cystitis. Distinguishing drug‑related damage from true lupus‑driven inflammation is crucial.
- Genetic and ethnic factors: The bulk of published cases come from Japan, Korea, China, and even Indonesia. While we can’t say genetics are the sole reason, there does seem to be a regional clustering that hints at HLA‑related susceptibility.
These causes aren’t mutually exclusive – many patients have a cocktail of autoantibodies, a history of immunosuppressive therapy, and a genetic backdrop that together set the stage for bladder trouble.
Lupus Cystitis Symptoms
Symptoms can be sneaky because they overlap with everyday problems. Here’s a quick cheat‑sheet to keep on hand:
| Urinary Signs | Non‑Urinary Signs |
|---|---|
| Dysuria (burning when you pee) | Abdominal or lower‑back pain |
| Frequency – up to 12+ trips/day | Nausea, vomiting, or diarrhea (often the first clue) |
| Nocturia – waking up multiple times at night | Fatigue, low‑grade fever, skin rash (malar rash) |
| Microscopic hematuria (blood you can’t see) | Joint pain, swelling, or other lupus flares |
| Urgency – “I have to go now!” feeling | Weight loss or unexplained anemia |
One particular symptom that trips people up is “increased need to urinate,” which can be mistaken for diabetes or a simple infection. If you notice that you’re drinking more water only to find yourself at the bathroom every 30‑45 minutes, it’s worth raising the question of lupus cystitis with your rheumatologist.
Lupus Cystitis Diagnosis
Diagnosing lupus cystitis is a bit like detective work – you need clues from labs, imaging, and sometimes a direct look inside the bladder.
- Blood work: Positive ANA, anti‑dsDNA, anti‑SSA/SSB, and low complement (C3, C4) support active SLE. A sterile urine culture helps rule out infection.
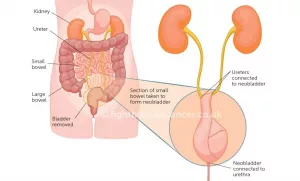
- Ultrasound: The first‑line imaging tool. It can show a thickened bladder wall (often >5 mm) and hydronephrosis—basically, backup of urine into the kidneys. A 2015 case report highlighted ultrasound as the key to spotting bilateral hydronephrosis in a lupus cystitis patient Urology Annals.
- CT or MRI: Used when ultrasound isn’t definitive or when you need to evaluate surrounding organs.
- Cystoscopy: Direct visualization can reveal diffuse erythema, ulcerations, and sometimes small bleeding spots. Biopsies, though rarely needed, show submucosal edema and perivascular lymphocyte infiltrates.
Putting these pieces together, most physicians will make a diagnosis of lupus cystitis when a patient with known SLE presents with compatible urinary symptoms, a sterile urine culture, and imaging that shows bladder wall changes or hydronephrosis.
Lupus Cystitis Treatment
Good news: with prompt treatment, most people see dramatic improvement. The main goal is to calm the immune system and protect the urinary tract from permanent damage.
- High‑dose steroids: Prednisone 1 mg/kg daily is the typical starting point. A rapid taper over 4‑6 weeks follows once symptoms improve.
- Cyclophosphamide pulses: Intravenous pulses (e.g., 0.5–1 g/m² monthly) have proven effective, especially when there’s concurrent lupus nephritis. The Chinese series showed over 80 % remission with this combo research.
- Mycophenolate mofetil (MMF) or azathioprine: Used for maintenance after initial steroid taper, particularly for patients who can’t tolerate cyclophosphamide.
- Biologics: In refractory cases, rituximab (anti‑CD20) has been reported to induce remission, though data are limited.
- Supportive care: Anticholinergic agents (e.g., oxybutynin) can curb urgency; bladder training exercises help regain normal capacity.
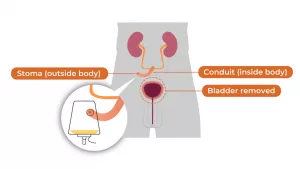
- Addressing hydronephrosis: If kidney swelling occurs, a temporary ureteric stent or percutaneous nephrostomy may be necessary until inflammation subsides.
Remember, medication decisions should always be personalized. Talk to a rheumatologist who understands both lupus and the urinary system – that dual expertise makes a world of difference.
Lupus Cystitis Risks
If left untreated, the inflammation can cause a cascade of problems:
- Hydroureteronephrosis: Swelling of the ureters and kidneys can lead to irreversible renal impairment.
- Bladder fibrosis: Chronic scarring reduces bladder capacity, leading to constant urgency or even urinary retention.
- Lupus enteritis overlap: About one‑third of patients experience simultaneous intestinal vasculitis, which can complicate nutrition and hydration.
- Pregnancy complications: Active lupus cystitis during pregnancy raises the risk of pre‑eclampsia and preterm birth; close monitoring is mandatory.
The silver lining? Early recognition and treatment usually prevent these long‑term sequelae. That’s why the “red‑flag” list below matters.
Living With Lupus
Now that we’ve tackled the medical heavy‑lifting, let’s talk about the day‑to‑day. Managing lupus cystitis isn’t just about pills; it’s a lifestyle.
- Bladder‑training schedule: Aim for 6–8 voids a day, spaced evenly. Keep a simple diary (time, volume, urgency level) to spot patterns.
- Hydration balance: About 1.5–2 L of water daily is ideal, unless your kidneys are compromised – then your doctor will tailor the amount.
- Diet tweaks: Cut back on bladder irritants like caffeine, carbonated drinks, and spicy foods. Some people find that a low‑acid, high‑fiber diet eases GI symptoms that often accompany cystitis.
- Gentle exercise: Walking, swimming, or prenatal yoga (if pregnant) improve circulation without jarring the bladder.
- Stress management: Mindfulness, deep‑breathing, or simply talking to a friend can lower overall lupus activity – stress is a known flare trigger.
- Regular follow‑up: Keep appointments with both your rheumatologist and urologist. Routine ultrasounds every 3–6 months help catch early hydronephrosis.
And don’t forget the emotional side. Living with a chronic, “invisible” condition can feel isolating. Joining a lupus support group—online or in‑person—gives you a place to share triumphs and frustrations. My buddy Maya swears by her weekly Zoom circle; she says hearing others’ stories “makes the pain feel less personal.”
Urgent Care Signs
If you notice any of the following, treat it like an emergency and call your doctor or go to the nearest ER:
- Sudden, severe flank pain or swelling
- Rapid rise in creatinine or loss of urine output
- Gross (visible) hematuria
- Fever >38 °C (100.4 °F) with chills
- Inability to empty the bladder despite the urge
Prompt intervention can save kidney function and prevent permanent bladder damage.
Trusted Resources Guide
When you’re digging for more information, stick to reputable sources:
- Lupus Foundation of America – patient education, support groups, and research updates.
- American College of Rheumatology (ACR) – clinical guidelines for SLE management.
- American Urological Association (AUA) – bladder health tips and professional directories.
These organizations keep their content up‑to‑date and backed by expert review, which aligns with Google’s “Helpful Content” guidelines – meaning the info you get is trustworthy, accurate, and truly useful.
So, there you have it. Lupus cystitis may be a rare and tricky condition, but armed with the right knowledge, you can spot it early, get the proper treatment, and live a life that feels normal again. If anything in this article sparked a question, drop a comment below or share your own experience – hearing from you makes the conversation richer for all of us.





















Leave a Reply
You must be logged in to post a comment.