So… Is the Worry Ever Really Gone?
Okay, real talk: Few things flip your whole world upside down like being told you need your bladder removed because of cancer. All those doctor appointments, anxiety before every scan… finally, the surgery is done. You surface from the haze determined to fight for normal again. Relief! But then, a quiet, nagging thought: Can bladder cancer return after bladder removal?
I’ll be honest, this question comes up a lot—online, in support groups, whispered late at night. You’re not weird for wondering. If anything, you’re totally normal for being a little bit scared… or maybe a lot.
Let’s dive right in, no sugarcoating. Because you deserve more than a pamphlet’s worth of answers—you deserve real talk, backed by what the experts and survivors have learned.
Why Does It Still Come Back?
Ghosts in the Machine: Bladder Cancer’s Tricky Side
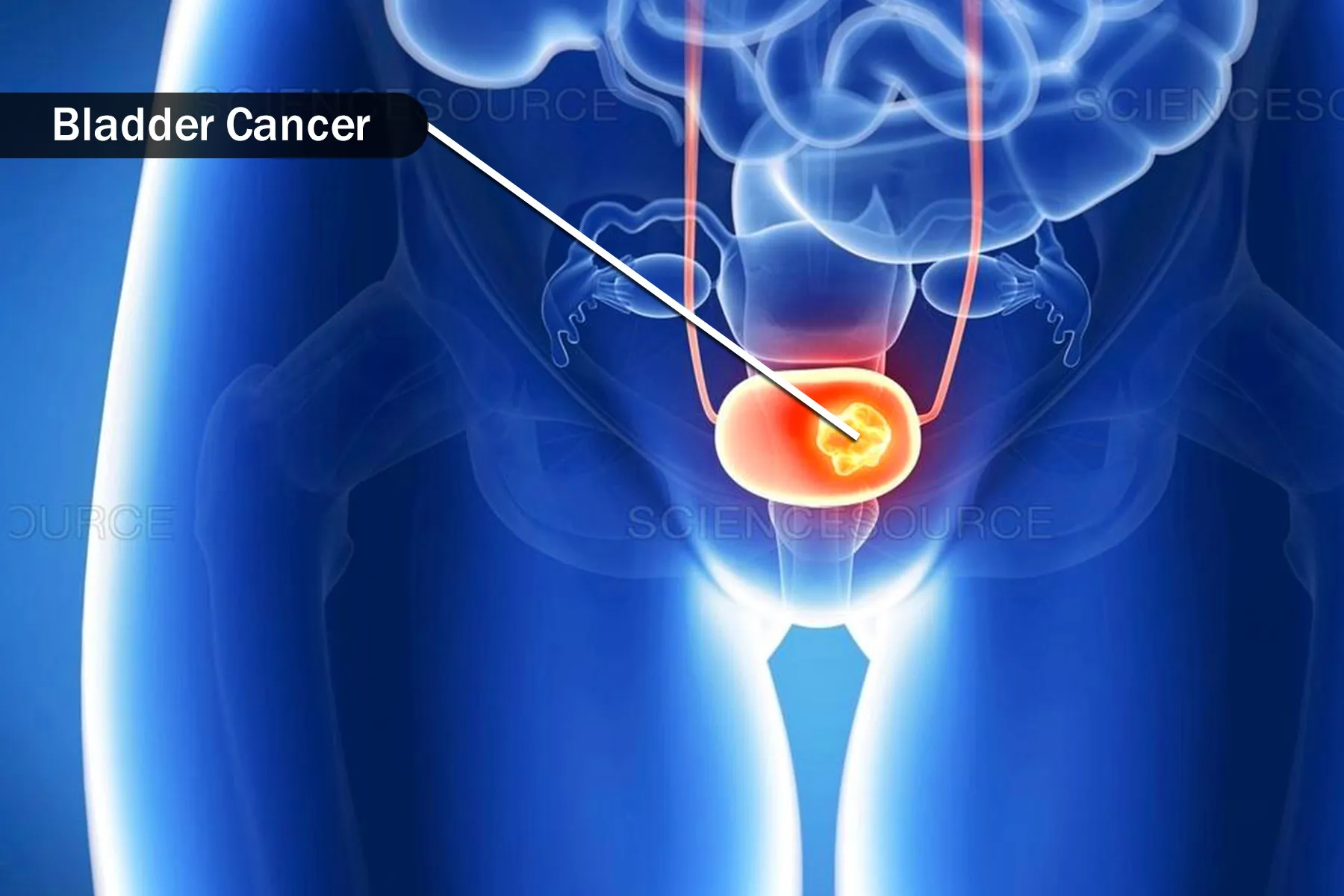
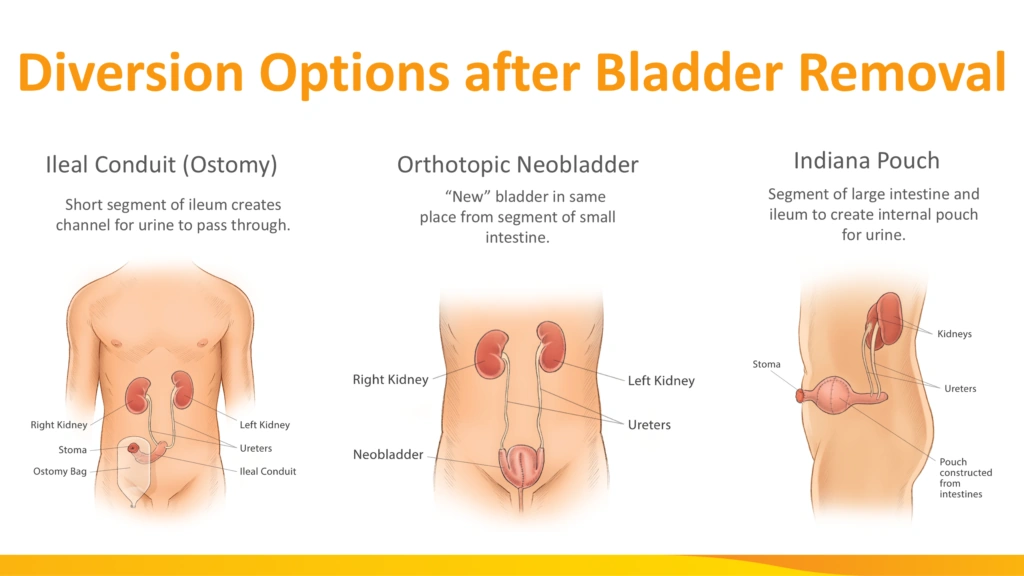
Here’s the frustrating part: yes, cancer can come back, even after the bladder is completely removed. This surgery is called a cystectomy—often a radical one, meaning the bladder, nearby tissue, and sometimes even more are taken out.
So why isn’t that the end of the story? Two words: tiny stragglers. Imagine you’ve cleaned your house top to bottom, but a couple stubborn dust bunnies hide behind the fridge. In the world of cancer, it’s not just about the visible tumor—sometimes there are microscopic cells hiding elsewhere, ready to stir up trouble months or years down the road.
Oh, and here’s the kicker: bladder cancer isn’t shy. According to research on bladder cancer recurrence and surveillance, recurrence rates after different treatments can run unsettlingly high—somewhere between 31% and 78% over five years, depending on stage and grade. Even after radical surgery, recurrence can pop up in about 30% to 50% of people according to early UK cancer center studies.
But… it’s not all grim. These are just numbers. What matters is what they mean for you.
What’s Actually Happening?
Cancer cells are sneaky little shape-shifters. Removing the bladder rids your body of the main “bad neighborhood,” but if a cell or two has already strayed—say, into a nearby lymph node, tissue outside the bladder, or even a bit of the urethra—well, that’s when can bladder cancer return after bladder removal goes from theory to reality. It’s like unplugging the stereo, but discovering one speaker’s still hooked up somewhere else.
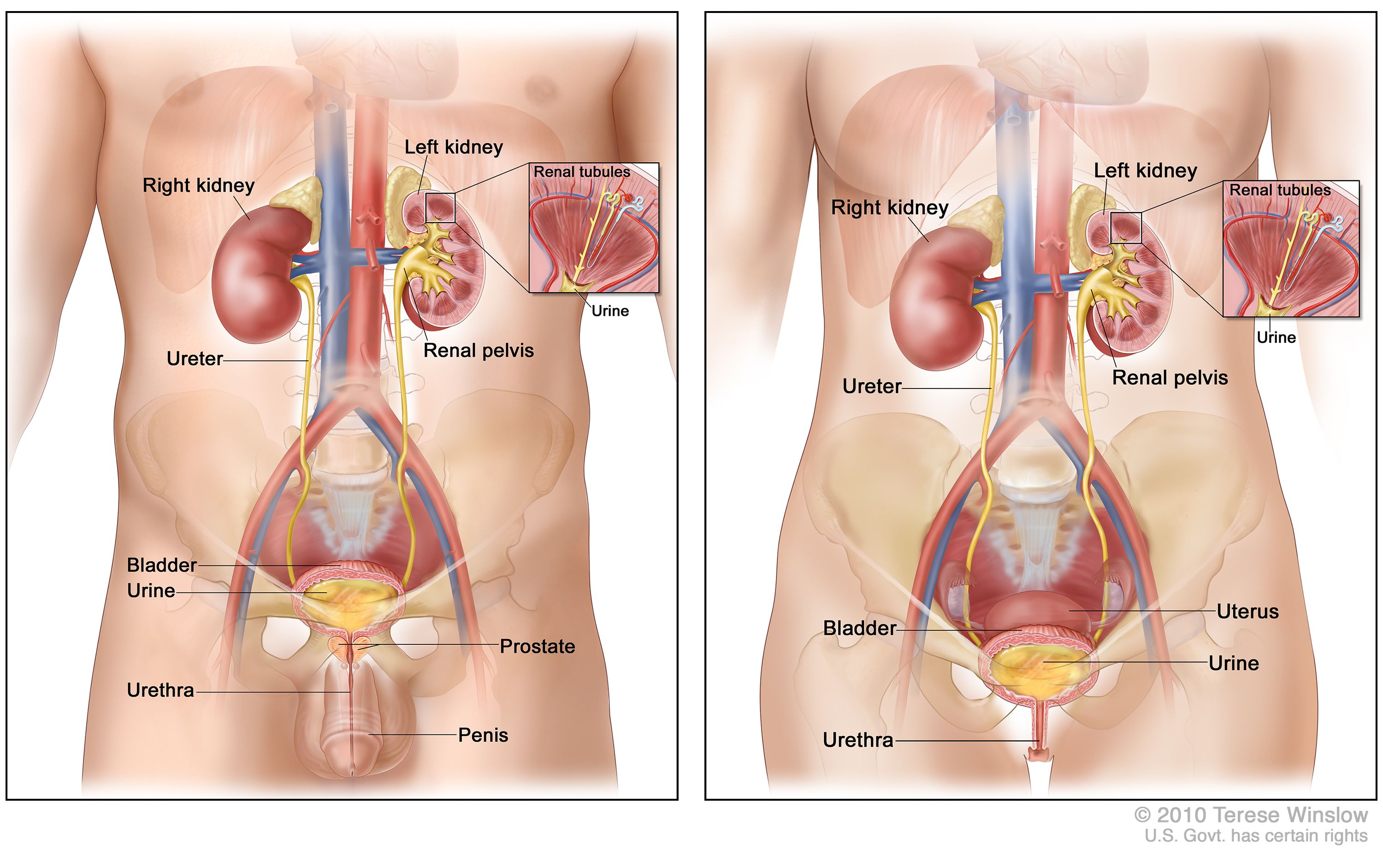
And get this: even years later, someone might hear the “music” again. In one rare case, a man developed cancer in his urethra twelve years after his bladder was removed. Twelve years! That’s a whole kid’s worth of time. But that’s rare—most recurrences, according to big studies, show up within the first two years, sometimes in the pelvis, sometimes further afield in places like the liver, bones, or lungs based on clinical guidelines.
:max_bytes(150000):strip_icc()/VWH_Illustration_Stages-of-Bladder-Cancer_Laura-Porter_Final-df3daf66b7f84175b9e13c6c86fd234d.jpg)
Quick Table: Where Can It Pop Up?
| Common Recurrence Sites | How Often It Happens | Timing |
|---|---|---|
| Lymph nodes (pelvic) | ~55% of recurrences | Usually within 14–18 months |
| Nearby pelvic tissue | ~45% | First 2 years common |
| Liver, bones, lungs | 10–19% (combined) | Variable—can be late |
| Urethra | 1–8% | Often within 2 years, but rare late cases |
Who’s Actually at Risk?
The Risk Recipe: It’s Not Just Luck
Ever played the game “guess who gets it”? Yeah, not fun with cancer. But certain patterns show up. Generally, the bigger and more aggressive your original cancer was, the higher your risk after surgery. Men have a slightly higher recurrence risk, especially if the original cancer was in the prostatic urethra (the little passage between bladder and outside). Also, advanced tumor stage—like T3 or T4—spells more trouble than earlier, confined stages.
Other things that muddy the waters: whether you smoked (I know, you’ve heard it all before…), if your margins were “clean” during surgery, and the number of cancer foci. Some studies even mention the surgical technique might matter for upper tract cancers, but honestly, there’s a lot we’re still learning based on a large analysis of risk factors.
And then… there’s genetics, weird chance, immune system quirks, maybe even something in the water? Not to get too “true crime podcast,” but cancer is unpredictable like that.
What Does the Timeline Look Like?
Most recurrences, experts say, show up early. Within the first two to three years is peak time—especially for muscle-invasive or advanced cases. On the other hand, it’s 100% possible to have nothing for a decade and then, out of nowhere, something new pops up. Don’t shoot the messenger. But also, don’t lose sleep every single night. That’s precious energy you need for living.
Which is why doctors are so big on check-ups. They want to catch anything before it spirals. If you want to nerd out on specifics, check this recent post about bladder cancer recurrence after 3 months for even more personal stories and numbers.
What Can You Actually Do? Monitoring, Detecting, Surviving
Surveillance Is Not Just for Spies
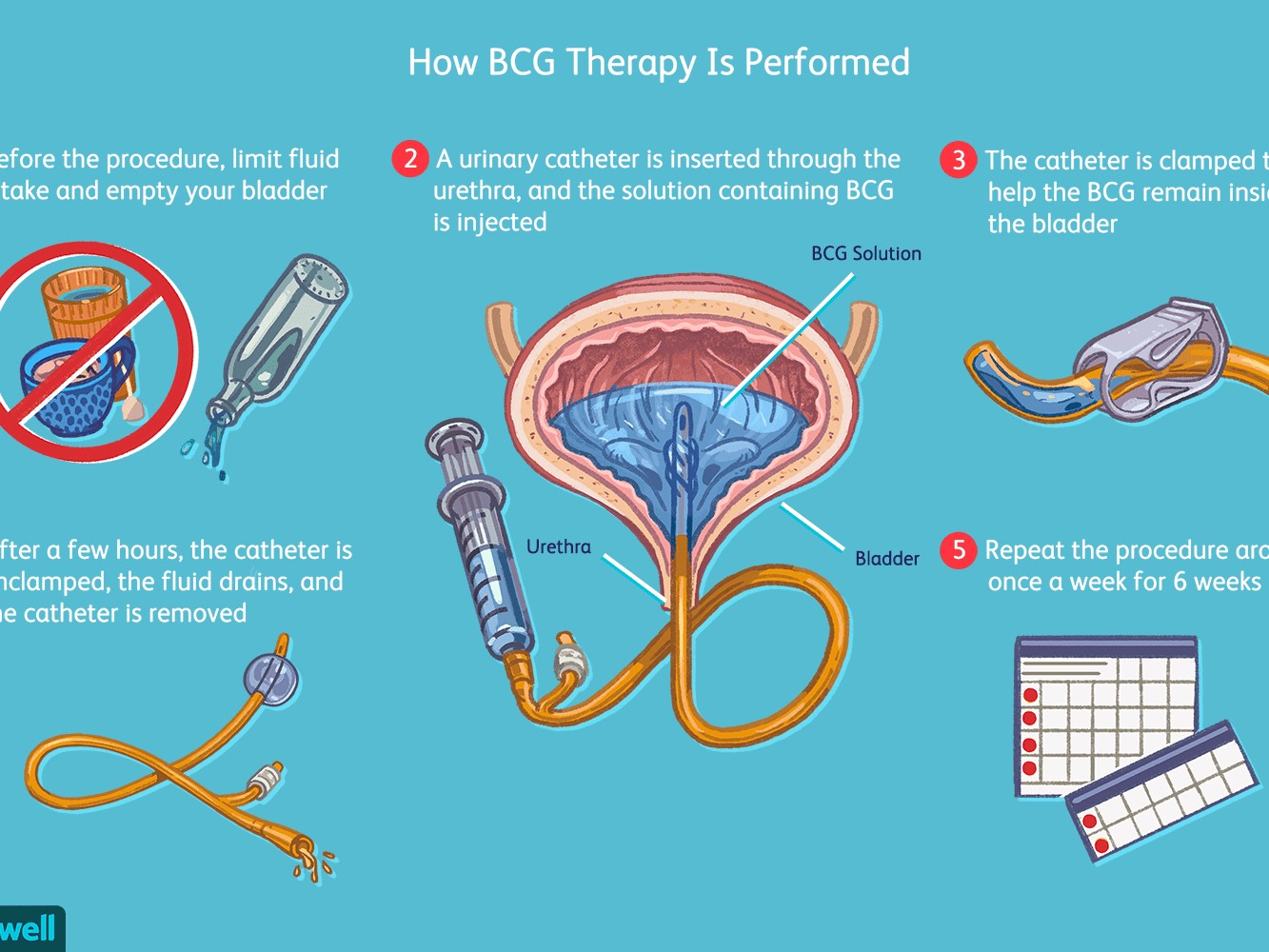
If you’re ever felt like your medical team is obsessed with poking and prodding—even years after surgery—now you know why!
Regular check-ins (surveillance) save lives. Think of it as detective work. Cystoscopies (little camera checks), urine tests, body scans—it’s all aimed at catching even a whisper of trouble before it gets loud. For high-risk folk, this schedule can run every 3–6 months at first, then space out over the years. It feels a bit over-the-top, but here’s the reality: early detection means you can stamp out a tiny problem rather than scramble once it’s bigger and meaner.
Almost like noticing a weird rattle in your car. You ignore it for a month…suddenly your whole engine’s coughing smoke on the highway. For cancer, the “sound” of recurrence can be as subtle as fatigue, some aches, blood in your urine (even a tiny bit), or—honestly—just a gut feeling something’s off. If in doubt? Pick up the phone. Your doctor’s used to “paranoid” calls. (Hint: They’re not really paranoid.)
Friend Moment: John’s Little Scare
I’ll pause for a quick story. John (let’s call him that), had his bladder out and life started normalizing. Then, nearly two years later, he felt off during a road trip. Not pain, just…weird. Turned out, a small recurrence in a pelvic node. Early catch meant quick treatment, and he’s back to fishing most weekends. True story—early checks matter.
Survival Numbers & Why They Don’t Tell the Whole Story
Numbers can be scary, but they’re just averages. Some muscle-invasive cancer folks see 50–80% cure rates after full removal—meaning, they never see the cancer again. Survival rates are pretty good for early-caught cancers (over 78% at 5 years by some reports), but they dip if disease was very advanced or spread before removal.
The more you’re on top of check-ups, the better your odds—plain and simple. It’s worth a look at the latest perspective on life expectancy after bladder removal for cancer if you want a more hopeful, practical take on what day-to-day life and survival really mean after surgery.
What If It DOES Come Back?
Huge sigh. If you’re here… or worried you might be… let’s talk next steps.
Not all recurrences are a death sentence. Localized returns might be fixed with another surgery or a bit of targeted therapy. If it spreads further, options expand: chemo, immunotherapy, radiation, or even promising new drugs. If you’re dealing with tough news, there’s always another path to try. And you’ve got specialists—urologists, oncologists, radiologists—fighting at your side.
Honestly, I’ve seen people go from panic to hope, then back to just plain living their lives. Like a friend who switched from chemo to immunotherapy and ended up joining a hiking group for survivors. It’s wild—the body and spirit bounce back in weird, lovely ways. That’s why those check-ups, even if annoying, are that bridge to hope.
How Should You Live With All This?
Living Beyond the Worry… Mostly
This is the part that never makes it into medical brochures. After all the surgery-scars, the scans, the good news, the “oh no, not again”—you’re supposed to somehow get back to living. But there’s always this “what if?” voice in the back of your mind.
No one can promise the worry disappears. But here’s the thing: so much of life after cancer is about learning to walk with the question, not letting it sit in the driver’s seat. You plan that trip. You hug your grandkids. You chase the cat off the kitchen counter (again). Some days, the “can bladder cancer return after bladder removal” question will try to mess with your head. But on most days, you’ll simply live.
It’s smart to keep an eye on the horizon. Stay curious and proactive—ask your doctor about a nomogram (it’s like a risk prediction tool just for you), take those calls seriously, and read up on current experiences like bladder cancer recurrence after 3 months so you remember you’re not weird (just human).
And if you ever feel adrift, it helps to revisit honest stories and practical “what now?” advice, like the community insights from life expectancy after bladder removal for cancer—they remind you the next chapter can be really, really good.
Wrapping Up: Let’s Walk This Road Together
Phew. If you’re still here, you deserve a high five. This topic isn’t light, but you’ve stuck with it—and that tells me plenty about your guts (pun intended? maybe). If you remember nothing else, let it be this: yes, bladder cancer can return after bladder removal, but you are not alone, and you are not powerless.
Your best defense? Show up for every single follow-up. Don’t ignore those tiny, weird symptoms. Lean on your care team—and even your fellow survivors. Pep yourself up with real-world stories (and, yes, memes if they help). Life is not about waiting for “the other shoe to drop”—it’s about grabbing every sunrise you can, statistics be damned.
So, can bladder cancer return after bladder removal? Yes. Will it dominate your joy? That part, you get to decide. I’m rooting for you—really. Now, get out there, live well, and let the “what ifs” shrink one ordinary, beautiful day at a time.

















Leave a Reply
You must be logged in to post a comment.