Hey there. If you’re reading this, you’ve probably felt that unsettling feeling that something isn’t quite right again, or maybe you’re just looking out for a friend. Either way, you deserve a clear, compassionate guide that cuts through the noise and hands you the early warning signs you need to spot a mental health relapse before it takes hold. Let’s sit together, sip that imaginary coffee, and walk through what to watch for, why it matters, and how a little self‑awareness and solid support can make all the difference.
Why It Matters
Imagine you’re driving down a familiar road and the brakes start to feel a little “spongy.” If you ignore that feeling, you might end up in a ditch. Relapse works the same way: it’s a gradual slide, not a sudden plunge. Missing the mental health relapse signs can lead to hospitalizations, deeper depression, or even dangerous cravings. On the flip side, catching those subtle cues early gives you a chance to press the brakes, call for help, and get back on track without the crash.
Studies from the National Institute on Drug Abuse show that at least one relapse is common for anyone dealing with chronic mental health conditions. The good news? Early detection can cut the length of a relapse by up to 50 % and dramatically improve long‑term recovery odds. So, the stakes are high, but the tools are within reach.
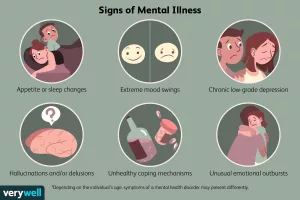
Core Early Signs
Below is a quick‑scan checklist you can keep on your phone, in your journal, or pinned to the fridge. When two or more of these pop up and linger for more than a week, consider it a red flag.
| Sign | What It Looks Like | Why It Matters |
|---|---|---|
| Mood Swings & Irritability | Sudden snap‑backs at small annoyances, feeling “on edge” most days. | Often the first emotional cue that your brain is re‑activating old stress pathways. |
| Sleep & Appetite Changes | Insomnia or oversleeping; eating far more or far less than usual. | Disrupted circadian rhythms can amplify anxiety and depressive thoughts. |
| Neglecting Self‑Care | Skipping showers, ignoring personal grooming, letting the living space become chaotic. | Self‑care is a barometer for how much emotional energy you have left. |
| Cognitive Fog | Trouble concentrating, forgetting appointments, feeling “spaced out.” | Brain fog often precedes a full‑blown mood episode. |
| Social Withdrawal | Canceling plans, avoiding friends, spending long periods alone. | Isolation removes the external reality checks that keep relapse at bay. |
| Rising Anxiety & Panic | Racing heart, shallow breathing, feeling “on the brink” without clear cause. | Anxiety fuels the urge to self‑medicate, nudging you toward relapse. |
| Romanticizing Past Behaviors | Day‑dreaming about “the good old days” when a substance or habit seemed comforting. | These thoughts can turn into justification for a slip. |
| Cravings or Urges | Sudden, strong desire to use a coping method you’d previously left behind. | Cravings are the mental stage of relapse—if unchecked, they become physical. |
These signs don’t appear in a vacuum. They’re often layered on top of everyday stressors—work, relationships, finances—so the key is to stay vigilant and treat each flag as a conversation starter with yourself or someone you trust.
Self Awareness Boost
Self‑awareness is like a mental flashlight: the brighter it shines, the less likely you are to trip over hidden obstacles. Below are a few gentle habits you can weave into daily life.
Daily Check‑In Worksheet
Grab a sticky note each morning and jot down three quick answers: “How do I feel?”, “What’s stressing me?”, “Did I notice any warning signs yesterday?” Review the notes weekly—patterns pop up fast when you write them down.
Journaling Prompts
Try these prompts when you feel “off”: “What triggered my irritability today?” “Did I skip any self‑care tasks? Why?” “Which thought kept looping in my head?” Honest answers help you catch the subtle mental drift before it becomes a tumble.
Mobile Mood‑Tracking Apps
Apps like Moodpath or Daylio let you log emotions with a single tap, then generate visual trends. The data is a neutral third party that can confirm (or refute) your gut feeling. Just remember to keep the app as a tool, not a crutch.
Support System Essentials
No one climbs a mountain solo, and the same goes for mental health recovery. A solid support group can spot the signs you miss while you’re in the thick of it.
The Power of a Support Group
When Gabe Howard, a podcast host and mental‑health advocate, opened up about his own recent relapse, he highlighted how his weekly peer group caught his early “energy dip” before it spiraled. According to Jor‑El Caraballo, LMHC, groups provide “real‑time accountability” and a shared vocabulary for describing those vague feelings.
Choosing the Right Group
- Size matters. 6‑10 members usually allow everyone a chance to speak.
- Facilitator credentials. Look for a licensed therapist or a trained peer‑leader.
- Frequency. Weekly meetings strike a good balance between consistency and burnout.
- Fit. Does the group discuss the specific condition you’re navigating? (e.g., depression, anxiety, bipolar).
Involving Professionals
Therapists, psychiatrists, and crisis lines are your safety net. If you notice three or more signs persisting for two weeks, call your therapist or hit 988 (US suicide & mental health helpline). It’s not “over‑reacting” — it’s proactive care.
Sample Script for Reaching Out
“Hey [Name], I’ve been feeling more irritable and my sleep’s been off lately. I’m worried it might be a sign I’m sliding back. Could we talk about what’s been going on?”
Prevention Strategies
Now that you know what to look for, let’s arm you with a toolbox of practical steps that keep relapse at arm’s length.
Structured Routine
Our brains love predictability. Set a morning ritual that includes a 10‑minute stretch, a brief meditation, and a quick glance at your daily checklist. Evening, wind down with a journal entry and a consistent bedtime.
Coping Toolbox
- Grounding 5‑4‑3‑2‑1. Name five things you see, four you hear, three you feel, two you smell, one you taste. It anchors you in the present.
- Box Breathing. Inhale 4 seconds, hold 4, exhale 4, hold 4. Repeats three times.
- Progressive Muscle Relaxation. Tighten each muscle group for five seconds, then release.
Medication Adherence
Whether it’s an antidepressant, mood stabilizer, or anti‑anxiety prescription, a simple pill‑box labeled by day prevents missed doses. If side effects bother you, talk to your prescriber—don’t self‑adjust.
Stress‑Management Plan
Identify your top three stress triggers (work, finances, relationship). For each, write a “Plan B” – a short activity you can do in five minutes (walk, call a friend, listen to a favorite song). The goal is to interrupt the cascade before it reaches a tipping point.
Emergency / Crisis Plan
Keep a one‑page sheet with:
- Names & numbers of two trusted contacts.
- The nearest emergency mental‑health clinic.
- Key medications you’re taking.
- A short “I’m feeling unsafe” statement you can text to a friend.
Having this plan printed and on your phone removes the decision‑making load when emotions run high.
When It Escalates
Sometimes the subtle signs evolve into a full‑blown relapse. Knowing the stages helps you act decisively.
Red‑Flag Escalation Timeline
Think of it as a three‑act play:
- Emotional Stage: Mood swings, irritability, anxiety.
- Mental Stage: Cravings, rationalizing the “need” to use, romanticizing past behaviors.
- Physical Stage: Actual substance use, severe sleep disruption, self‑harm thoughts.
If you recognize yourself moving from stage 1 to stage 2, hit your support network immediately. If stage 3 appears, call emergency services—your safety is the priority.
Immediate Actions
- Notify a trusted person. Share exactly what you’re experiencing.
- Remove temptations. Put away any substances, medications, or triggers.
- Engage in a grounding technique. Box breathing for two minutes.
- Seek professional help. Schedule an urgent appointment or go to the nearest crisis center.
Wrapping It All Up
Spotting mental health relapse signs isn’t about being hyper‑vigilant to the point of paranoia; it’s about cultivating a gentle awareness that lets you intervene before a small wobble becomes a tumble. The checklist, self‑awareness habits, supportive community, and prevention toolbox we’ve explored are all pieces of the same puzzle. When they fit together, you create a sturdy safety net for yourself—or for the loved ones you care about.
Remember: you’re not alone, and you don’t have to go it alone. If any of the signs above feel familiar, take a moment now—pick up the phone, write a note, or simply breathe deeply. A tiny step today can keep a larger setback far away.
What’s one early warning sign you’ve noticed in yourself or a friend? Share it in the comments—your story could be the lifeline someone else needs.























Leave a Reply
You must be logged in to post a comment.