Ever wondered who’s behind the tiny black dots you see on a blood‑test report, or why a doctor can tell if a lump is cancer just by looking at a slice of tissue? That invisible hero is the pathologist. In plain English, pathologists are doctors who study body tissues, cells and fluids to diagnose disease, guide treatment, and keep the rest of the health‑care team on solid ground. Their work touches almost every lab test you ever get – from a routine cholesterol check to a life‑changing cancer biopsy – and knowing what they do can make the whole medical journey feel a lot less mysterious.
How Pathology Works
Pathology is literally “the study of disease.” It splits into two big camps: anatomical pathology, which looks at solid tissues and organs, and clinical pathology, which analyses blood, urine, and other body fluids. Both camps use microscopes, stains, molecular probes, and sometimes even AI‑driven image analysis to turn a tiny specimen into a clear diagnosis.
According to the Royal College of Pathologists of Australasia, roughly 75 % of all medical decisions rely on pathology and laboratory information. That’s a staggering number – it means every time your doctor decides on a medication, a surgery, or a monitoring plan, a pathologist’s work is the foundation.
Think of pathology as the “doctor’s doctor.” Surgeons, oncologists, primary‑care physicians, and even dentists lean on pathologists for the definitive answer to “what’s really going on inside the body?” Without that answer, treatment would be guesswork.
Core Pathology Duties
While the exact duties shift a bit from one specialty to another, most pathologists share a core set of responsibilities:
- Examining tissue samples (histopathology) – Biopsies, surgical resections, and autopsy specimens are sliced, stained, and examined under a microscope to spot disease.
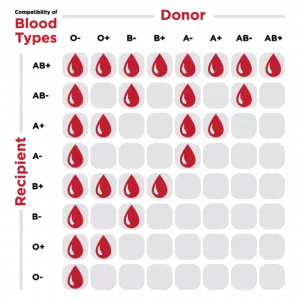
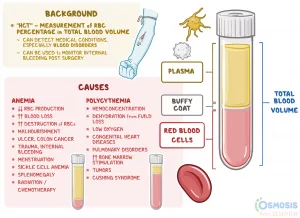
- Analyzing blood and body fluids (clinical chemistry & haematology) – From a simple CBC to complex hormone panels, these results steer everything from emergency care to chronic disease management.
- Microbiology & infection work‑up – Culturing bacteria, running PCR tests, and identifying drug‑resistant bugs keep infections in check.
- Providing consults and interpreting results – Pathologists often talk directly with clinicians, clarifying what a result really means for a patient’s next step.
- Ensuring lab quality and safety – They oversee accreditation, internal quality control, and proficiency testing, making sure the lab’s “answers” are reliable.
- Research, teaching & policy advising – Many split their time between patient care and advancing the science, writing guidelines, or mentoring the next generation of doctors.
Pathology Specialties Overview
The field is surprisingly diverse. Below is a quick snapshot of the most common specialties, what they examine, and where you’ll usually find them.
| Specialty | Typical Samples | Common Settings |
|---|---|---|
| Anatomical Pathology | Biopsy tissue, surgical resections, autopsy organs | Hospital labs, university medical centers |
| Clinical (Chemical) Pathology | Blood, urine, cerebrospinal fluid | Community hospitals, commercial labs |
| Haematology | Whole blood, bone‑marrow aspirates | Specialist blood labs, oncology units |
| Microbiology & Virology | Swabs, cultures, tissue homogenates | Infection‑control labs, public‑health labs |
| Immunopathology | Serum, tissue sections for immune markers | Transplant centers, autoimmune clinics |
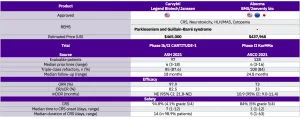
| Genetic / Molecular Pathology | DNA/RNA extracts, tumor panels | Precision‑medicine labs, research institutes |
| Forensic Pathology | Whole bodies, organ fragments | Coroner offices, law‑enforcement labs |
The list isn’t exhaustive – there are also niche areas like toxicology, veterinary pathology, and ophthalmic pathology – but it captures the breadth of “pathology specialties” you might have heard about.
A Day in Lab
Let’s walk through a typical day for a few different pathologists. Picture this as a backstage pass to the medical world.
Hospital‑based Anatomical Pathologist
At 7 a.m. the pathologist receives a “frozen section” request: a surgeon just removed a mysterious brain lesion and needs to know whether it’s cancer before deciding on the next step. Within minutes, the tissue is sliced, stained, and examined under a high‑resolution microscope. The pathologist shouts “malignant!” over the intercom, allowing the surgeon to proceed with an aggressive resection while the patient is still in the operating room. It’s high‑stakes, high‑impact, and the result is delivered in real time.
Clinical Pathologist in a Community Lab
Meanwhile, a clinical pathologist at a suburban medical center spends the morning reviewing a batch of liver‑function panels. One result shows a dramatically elevated ALT and AST. He calls the ordering primary‑care physician, explains the likely cause (possible medication‑induced liver injury), and advises an immediate medication review. The patient avoids a potential hospital admission – all because the pathologist interpreted the numbers and communicated promptly.
Forensic Pathologist
On a rainy Thursday, a police detective brings in a body recovered from a construction site. The forensic pathologist conducts an autopsy, documenting the injuries, collecting tissue for toxicology, and ultimately concluding the cause of death was blunt‑force trauma rather than a drug overdose. The findings shape the subsequent criminal investigation and bring closure to the victim’s family.
Pathology Researcher & Teacher
In the afternoon, an academic pathologist supervises graduate students in a molecular‑genetics lab, guiding them through a new assay that detects a rare KRAS mutation in pancreatic cancer. The same day, she delivers a short lecture to fourth‑year medical students, using a real case she handled last week to illustrate how molecular results guide targeted therapy. Her dual role keeps the pipeline from bench to bedside humming.
These snapshots illustrate the “experience” side of pathology – real‑world problem solving, rapid decision‑making, and a genuine impact on patient lives.
Pathology Career Path
If you’re drawn to the detective work of medicine, pathology might feel like a perfect fit. Here’s a step‑by‑step look at how you can become one:
- Medical school (4‑5 years) – Earn an MBBS/MD, covering anatomy, physiology, and clinical rotations.
- Residency in pathology (minimum 5 years) – Includes basic pathological sciences (BPS) exams, rotations through anatomical, clinical, and laboratory sections. According to the Royal College of Pathologists, the BPS exam is a key milestone.
- Fellowship (optional, 1‑2 years) – Specialize in histopathology, molecular genetics, forensic pathology, or any of the other “pathology specialties” listed above.
- Board certification – In the U.S., the American Board of Pathology; elsewhere, the Royal College or equivalent. Recertification occurs every 10 years (see Hopkins).
- Career options – Hospital labs, private diagnostic companies, academic research, governmental health agencies, or even consulting for biotech firms.
Salary ranges vary: a junior pathology resident earns around $60 k USD annually, while a senior consultant in a major university hospital can pull $300 k USD or more (source: Prospects 2025). The field also offers a relatively stable work‑life balance compared with many front‑line specialties, especially for those who prefer lab‑based work.
Benefits and Risks
Like any medical discipline, pathology has bright spots and shadowed corners.
Benefits
- Accurate, objective diagnosis – Pathologists provide the gold‑standard evidence for treatment decisions.
- Early disease detection – Screening programs (e.g., newborn metabolic panels) rely on precise lab results.
- Broad impact – A single tissue diagnosis can affect surgery, chemotherapy, and long‑term follow‑up for dozens of patients.
Potential Risks / Limitations
- Sample quality – Poorly collected or mishandled specimens can lead to misdiagnosis.
- Turn‑around‑time pressure – Emergency cases demand results within hours; delays may compromise care.
- Technology reliance – Over‑reliance on automated platforms without clinical context can produce false‑positive or false‑negative findings.
Pathologists mitigate these risks through rigorous quality‑control programs, double‑sign‑off policies, and constant communication with clinicians (as highlighted in the Royal College of Pathologists’ position statement).
Real World Stories
Stories stick. Here are two short anecdotes that show why understanding “pathologists and pathology” matters to everyday folks.
The Unexpected Diagnosis
Maria, a 45‑year‑old teacher, went in for a routine blood test after feeling unusually tired. The clinical pathologist noticed a subtle, yet consistent, elevation in her serum calcium and ordered a parathyroid hormone assay. The results pointed to a tiny, otherwise asymptomatic parathyroid adenoma. Early surgery, guided by the pathologist’s interpretation, cured Maria before she ever experienced a kidney stone or bone pain. She now tells friends, “If it weren’t for the lab whisperer, I’d still be wondering why I was always exhausted.”
From Biopsy to Hope
When 62‑year‑old James had a lump removed from his colon, the surgeon sent the tissue to an anatomical pathologist. The histopathology report revealed early‑stage adenocarcinoma with clear margins, meaning the cancer hadn’t spread beyond the tissue slice. Thanks to that precise tissue analysis, James received a brief course of chemotherapy and is now cancer‑free. He credits the “microscope magician” for turning a scary diagnosis into a survivable story.
These narratives illustrate the human side of pathology – it isn’t just slides and numbers; it’s about real people, real outcomes, and often, real relief.
Useful Resources for Readers
If you want to dig deeper, these sources are trustworthy and written by experts:
- Royal College of Pathologists – Careers in Pathology
- Johns Hopkins – What Is a Pathologist?
- Prospects – Pathologist Job Profile (2025 data)
- RCPA – What Is Pathology?
These links are sprinkled throughout the article, so you can explore any point that piques your curiosity without losing the flow of reading.
Conclusion
Pathologists may wear white coats and spend most of their time behind a microscope, but their influence reaches every corner of modern medicine. From the moment a tiny drop of blood is drawn to the final decision about surgery, they turn mystery into clarity. Understanding their duties, specialties, and the rigorous training that shapes them not only demystifies the lab reports you receive but also helps you become a more informed patient or a future colleague.
So the next time you glance at a lab result, remember the pathologist who turned a speck of tissue into a life‑changing answer. If you’ve ever wondered about a particular test, feel free to ask your doctor, “What did the pathologist find?” – you’ll be tapping into a vital part of the health‑care team that’s often hidden in plain sight.
What’s your experience with pathology? Have you ever received a diagnosis that hinged on a tissue slice or a blood panel? Share your story in the comments; let’s keep the conversation going!




















Leave a Reply
You must be logged in to post a comment.