Stress is the #1 trigger for psoriasis flare‑ups, but it isn’t the only one. When worry, deadlines, or even a traffic jam crank up your body’s stress hormones, the immune system goes into overdrive, skin cells multiply faster, and those red, scaly patches pop back up.
In the next few minutes you’ll learn exactly how stress fuels those flares, discover the other big psoriasis triggers, and walk away with a simple, step‑by‑step stress‑management plan you can start today. Grab a cup of tea, get comfortable, and let’s dive in together.
Why Stress Matters
How stress hijacks the immune system
Think of your immune system as a busy newsroom. Under normal conditions it prints the headlines you need—fighting infections, repairing tissue. Stress is like a rogue editor that shouts “More! More! More!” and the newsroom floods the pages with pro‑inflammatory cytokines such as IL‑17, TNF‑α, and IL‑22. Those chemicals are the same culprits that create the thick plaques characteristic of psoriasis.
According to a 2023 article on Verywell Health, stress elevates these cytokines, and higher cytokine levels are directly linked to more severe flare‑ups.
The cortisol paradox – low baseline, high spikes
Most of us think cortisol is the “bad guy” that makes us anxious, but for people with psoriasis it’s a bit more complicated. Research shows that many patients have lower resting cortisol levels, which means their bodies have fewer natural anti‑inflammatory brakes. When a stressful event hits, cortisol spikes sharply but never reaches the level needed to calm the inflammation.
Dr. Evan Rieder, a dermatologist at NYU Langone Health, explains in Healthline that this impaired cortisol response creates a perfect storm for flare‑ups.
Neuro‑genic inflammation – nerves, SP & NGF
Stress also talks to your skin through nerves. When you’re stressed, nerves release neuropeptides like substance P (SP) and nerve growth factor (NGF). These messengers summon immune cells to the skin, turning a calm surface into a battlefield.
A 2024 study presented at the European Academy of Dermatology and Venereology (EADV) found that just 24 hours of “sonic” stress caused psoriasis lesions to relapse in every human skin xenograft examined (News‑Medical).
Full Trigger List
Stress may be the headliner, but many other factors can pull the curtain on a flare. Below is a quick‑look table that shows how each trigger interacts with stress and a tiny tip you can try right now.
| Trigger | How It Fuels Flares | Simple Mitigation Tip |
|---|---|---|
| Infections (strep, skin fungi) | Activate immune pathways already primed by stress | Stay up‑to‑date on vaccinations and treat infections promptly |
| Cold, dry weather | Dry skin worsens inflammation, stress often spikes in winter | Use a fragrance‑free moisturizer twice daily |
| Medications (beta‑blockers, lithium) | Alter immune signaling, can compound stress‑induced cytokines | Discuss alternatives with your doctor |
| Alcohol & smoking | Raise systemic inflammation, increase cortisol spikes | Swap one drink for a non‑alcoholic mocktail this week |
| Stress (emotional/physical) | Raises pro‑inflammatory cytokines & neuropeptides | 5‑minute breathing exercise before bed |
Spotting Early Signs
Physical cues
When stress is about to launch a flare you might notice:
- A sudden increase in the number of plaques
- Itching that feels “off‑scale” intense
- Plaques becoming thicker or more erythematous (red)
Emotional/behavioral cues
Stress isn’t always obvious. You might feel:
- Restlessness or a racing mind
- Sleep drifting off after midnight
- A vague “tightness” in your chest or throat
When you catch these signs early, you can intervene before the flare spreads.
Effective Stress Management
Mindfulness & meditation (quick starter)
Close your eyes. Inhale for a count of four, hold two, exhale four. Do this for five minutes. It sounds simple, but studies show regular mindfulness can lower cortisol and, in turn, reduce flare frequency.
Physical activity that doesn’t aggravate skin
Low‑impact cardio—think brisk walking, stationary cycling, or a gentle yoga flow—keeps blood flowing, releases endorphins, and helps regulate the HPA‑axis (the stress‑hormone system). Aim for 30 minutes most days; you’ll notice calmer skin and a clearer mind.
Cognitive‑behavioral therapy (CBT) & professional help
When thoughts turn into a loop of “my skin will never improve,” CBT can re‑wire that pattern. A therapist trained in chronic‑illness care can teach you coping tools that directly cut down the stress‑flare cycle.
Lifestyle tweaks that cut stress + flare risk
- Sleep hygiene: 7–9 hours, dark room, no screens 30 min before bedtime.
- Balanced diet: Omega‑3 rich fish, leafy greens, and plenty of water fight systemic inflammation.
- Limit alcohol & caffeine: Both can spike cortisol.
- Gentle skin care: Lukewarm showers, fragrance‑free cleansers, and a good moisturizer seal the skin barrier.
Mini‑checklist (copy‑paste ready)
- ☑️ 5‑minute breathwork each morning
- ☑️ 20‑minute walk after lunch
- ☑️ Journal stress triggers before bed
- ☑️ Apply moisturizer within 3 minutes of shower
- ☑️ Schedule a 30‑minute “no‑screen” unwind time
Medical Options Overview
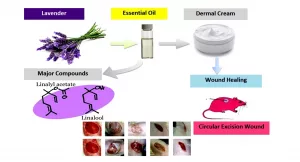
Topical treatments during a stress‑flare
When a flare hits, fast‑acting topicals like corticosteroids or vitamin D analogues can calm the inflammation while you work on stress‑reduction. Use them exactly as your dermatologist advises—usually once or twice daily on affected spots.
Systemic & biologic therapies
For moderate‑to‑severe disease, doctors may prescribe oral meds (methotrexate, apremilast) or biologics that target specific cytokines (IL‑17, IL‑23). These drugs essentially turn down the volume on the cytokine “storm” that stress amplifies.
Integrating stress‑management with medical care
Tell your dermatologist about the stress triggers you’ve identified. A collaborative plan—medical treatment plus a concrete stress‑relief routine—has been shown to improve outcomes and quality of life.
Quick‑Start Action Plan
Ready to put theory into practice? Here’s a 7‑day “stress‑free” challenge that blends mindfulness, movement, and skin‑care.
- Day 1: Download a free guided breathing audio and do a 5‑minute session before bed.
- Day 2: Start a simple journal. Write down every stressful moment and any skin changes you notice.
- Day 3: Take a 20‑minute walk outdoors. Notice the sounds, the breeze, the sunlight.
- Day 4: Swap your afternoon coffee for green tea (rich in antioxidants).
- Day 5: Stretch for 10 minutes before sleep—helps release muscle tension.
- Day 6: Reach out to a friend or join an online psoriasis support group for a quick chat.
- Day 7: Review your journal. Did any flare appear? Adjust your routine for next week.
Feel free to print this list or save it on your phone. Consistency is the secret sauce.
Conclusion
Stress is a powerful, measurable trigger for psoriasis flares, but it’s not a destiny you have to accept. By understanding the biology—how stress hormones, cytokines, and neuropeptides interact—you can spot early warning signs, avoid other common triggers, and apply a blend of proven stress‑relief techniques alongside your medical regimen.
When you combine a thoughtful skin‑care routine with simple habits like mindful breathing, daily movement, and a supportive community, you break the vicious cycle and give your skin the chance to heal. Have you tried any of these strategies? What worked best for you? Share your story in the comments or download the 7‑day challenge PDF and start your own journey to calmer skin today.























Leave a Reply
You must be logged in to post a comment.