Subacute cutaneous lupus (SCLE) is a form of lupus that produces skin eruptions. It’s often provoked by sunlight and can be induced or aggravated by certain drugs, including proton pump inhibitors and calcium channel blockers.
SCLE is one subtype of cutaneous lupus erythematosus (CLE). CLE primarily involves the skin, producing rashes and lesions that can be painful or itchy. SCLE represents about 8% of CLE cases.
While SCLE can develop in anyone, it appears more frequently in some groups, particularly women. Around half of people with SCLE also have systemic lupus erythematosus (SLE). Some individuals with SCLE later develop full SLE.
SLE is an inflammatory condition in which the immune system mistakenly attacks healthy tissues and organs, potentially affecting the kidneys, heart, lungs, or nervous system.
SCLE is linked with other disorders as well, such as Sjögren disease. Continue reading to learn more about SCLE, including its signs, triggers, and management options.
What is subacute cutaneous lupus?
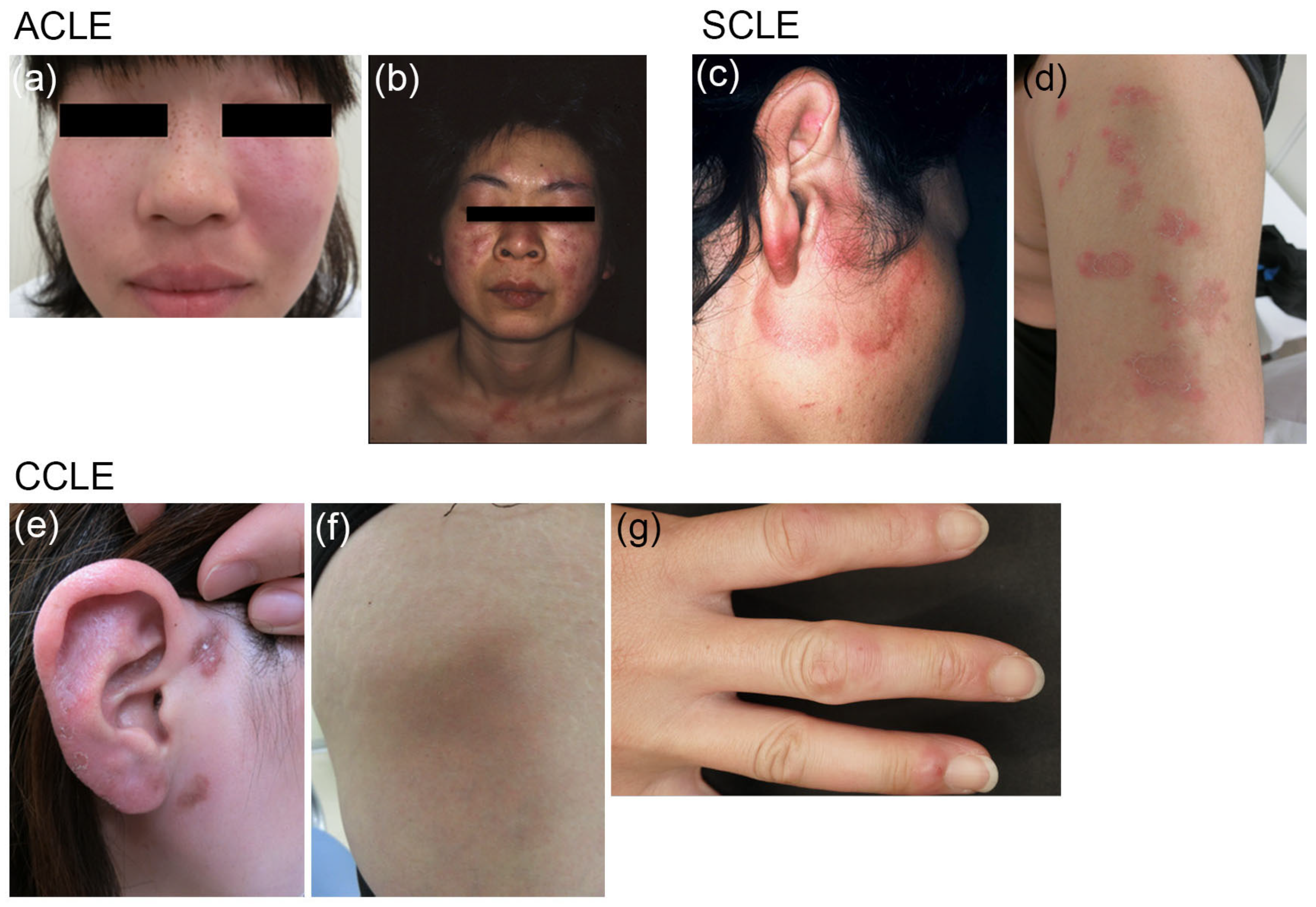
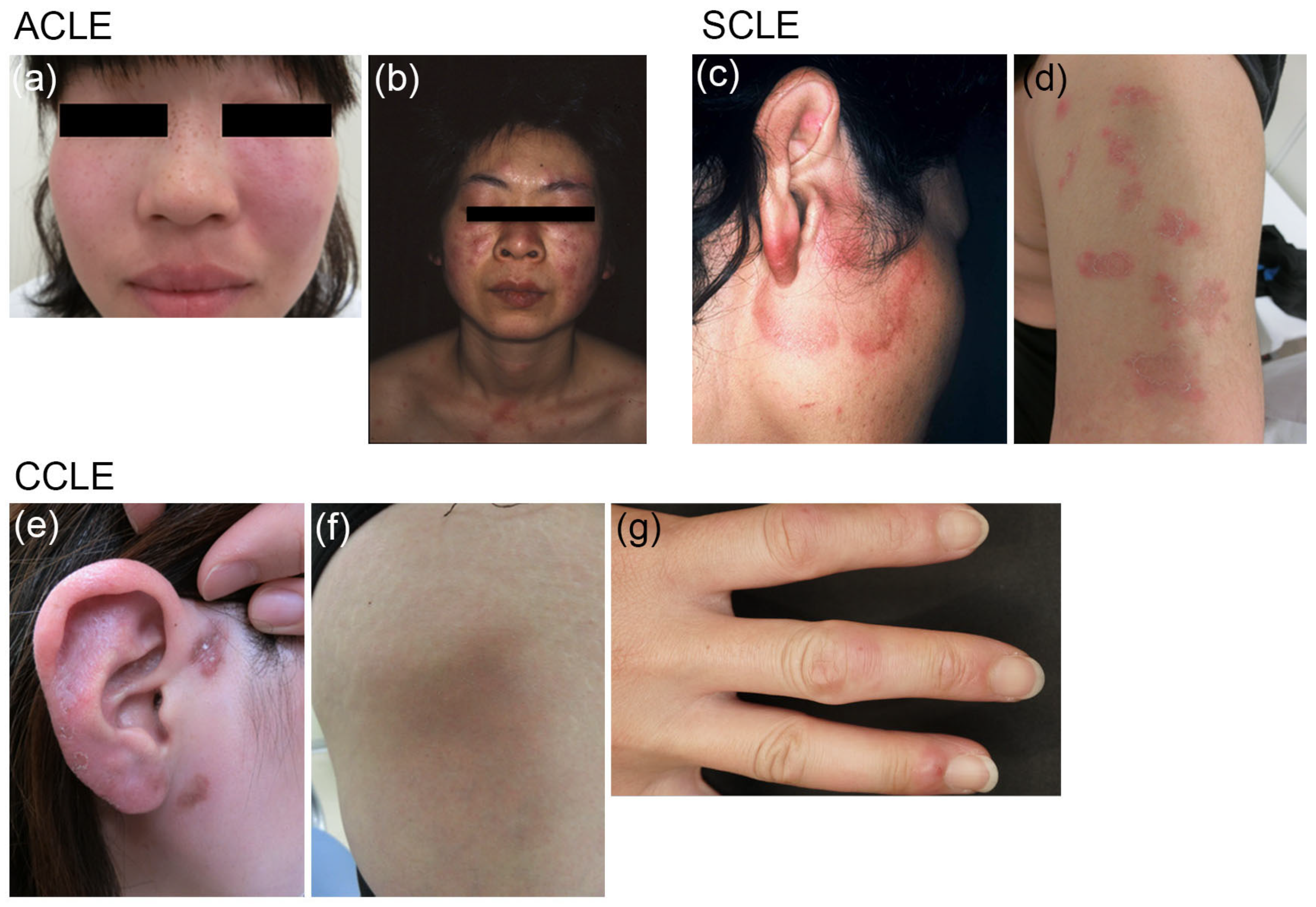
SCLE is a subtype of CLE and can occur in people who have systemic lupus (SLE). That means someone might first present with an SCLE rash and later develop non-skin SLE symptoms, like kidney involvement. Other CLE varieties include:
- acute cutaneous lupus
- chronic cutaneous lupus
SCLE mainly affects the skin, producing annular (ring-shaped) sores, patches, or rashes that may be painful or pruritic. These lesions can appear red on lighter skin and may look purple or dark brown on darker skin tones. Unlike chronic cutaneous lupus, SCLE generally does not leave scars or permanent textural changes.
SCLE differs from acute cutaneous lupus, which is typified by a rash that spans both cheeks and the bridge of the nose — commonly referred to as a “butterfly” or malar rash. That mildly raised rash often appears red on pale skin or purple/dark brown on darker complexions.
Rashes from SCLE usually spare the face and scalp, appearing instead on the trunk, back, arms, or chest.
These rashes can also surface during an SLE flare.
What are the symptoms of subacute cutaneous lupus?
Typical SCLE signs include rashes on areas of the body exposed to sunlight, such as the arms, back, chest, or torso. The lesions may present as:
- ring-shaped
- swollen
- red
- purple
- dark brown
- bumpy
- dry
After the rash resolves, some people may notice transient changes in skin pigmentation.
What causes subacute cutaneous lupus?
SCLE can arise independently or as part of SLE. It may also be drug-induced after prolonged exposure to certain medications, including calcium channel blockers or proton pump inhibitors.
Drugs are estimated to trigger roughly one-third of SCLE instances. Symptoms can begin months to years after starting the implicated medication. Examples include:
- pantoprazole
- omeprazole
- nifedipine
- diltiazem
- terbinafine
Other medicines reported to precipitate SCLE include:
- antihypertensives such as diuretics or angiotensin-converting enzyme inhibitors
- antifungal agents
- anticonvulsant drugs
- statins
- antihistamines
- antibiotics
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- chemotherapy medications
- biologic immunotherapies
- antidepressants
Environmental exposures, notably ultraviolet light, also increase the likelihood of flares.
How does a doctor diagnose subacute cutaneous lupus?
A specialist such as a dermatologist or rheumatologist usually makes the diagnosis. During evaluation, they will ask about your:
- <
- acute cutaneous lupus
- chronic cutaneous lupus
- ring-shaped
- swollen
- red
- purple
- dark brown
- bumpy
- dry
- pantoprazole
- omeprazole
- nifedipine
- diltiazem
- terbinafine
- antihypertensives such as diuretics or angiotensin-converting enzyme inhibitors
- antifungal agents
- anticonvulsant drugs
- statins
- antihistamines
- antibiotics
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- chemotherapy medications
- biologic immunotherapies
- antidepressants
- symptoms
- medical history
- family history
- medication use
- urinalysis
- blood tests to detect specific proteins or antibodies
- skin biopsy to analyze a sample of affected tissue
- lupus band test, which examines a specimen of seemingly unaffected skin
- dapsone
- thalidomide
- interferon
- systemic retinoids
- immunosuppressive agents
Subacute cutaneous lupus (SCLE) is a form of lupus that produces skin eruptions. It’s often provoked by sunlight and can be induced or aggravated by certain drugs, including proton pump inhibitors and calcium channel blockers.
SCLE is one subtype of cutaneous lupus erythematosus (CLE). CLE primarily involves the skin, producing rashes and lesions that can be painful or itchy. SCLE represents about 8% of CLE cases.
While SCLE can develop in anyone, it appears more frequently in some groups, particularly women. Around half of people with SCLE also have systemic lupus erythematosus (SLE). Some individuals with SCLE later develop full SLE.
SLE is an inflammatory condition in which the immune system mistakenly attacks healthy tissues and organs, potentially affecting the kidneys, heart, lungs, or nervous system.
SCLE is linked with other disorders as well, such as Sjögren disease. Continue reading to learn more about SCLE, including its signs, triggers, and management options.
What is subacute cutaneous lupus?
SCLE is a subtype of CLE and can occur in people who have systemic lupus (SLE). That means someone might first present with an SCLE rash and later develop non-skin SLE symptoms, like kidney involvement. Other CLE varieties include:
SCLE mainly affects the skin, producing annular (ring-shaped) sores, patches, or rashes that may be painful or pruritic. These lesions can appear red on lighter skin and may look purple or dark brown on darker skin tones. Unlike chronic cutaneous lupus, SCLE generally does not leave scars or permanent textural changes.
SCLE differs from acute cutaneous lupus, which is typified by a rash that spans both cheeks and the bridge of the nose — commonly referred to as a “butterfly” or malar rash. That mildly raised rash often appears red on pale skin or purple/dark brown on darker complexions.
Rashes from SCLE usually spare the face and scalp, appearing instead on the trunk, back, arms, or chest.
These rashes can also surface during an SLE flare.
What are the symptoms of subacute cutaneous lupus?
Typical SCLE signs include rashes on areas of the body exposed to sunlight, such as the arms, back, chest, or torso. The lesions may present as:
After the rash resolves, some people may notice transient changes in skin pigmentation.
What causes subacute cutaneous lupus?
SCLE can arise independently or as part of SLE. It may also be drug-induced after prolonged exposure to certain medications, including calcium channel blockers or proton pump inhibitors.
Drugs are estimated to trigger roughly one-third of SCLE instances. Symptoms can begin months to years after starting the implicated medication. Examples include:
Other medicines reported to precipitate SCLE include:
Environmental exposures, notably ultraviolet light, also increase the likelihood of flares.
How does a doctor diagnose subacute cutaneous lupus?
A specialist such as a dermatologist or rheumatologist usually makes the diagnosis. During evaluation, they will ask about your:
The clinician will examine your skin for characteristic rashes and lesions. Additional tests that may be ordered include:
What are the treatment options for subacute cutaneous lupus?
Managing SCLE typically combines lifestyle measures and medications when needed. Because sunlight commonly triggers SCLE, limiting sun exposure is essential to prevent or reduce symptoms.
When outdoors, use a broad-spectrum sunscreen with at least SPF 50 and wear sun-protective clothing such as a wide-brimmed hat. For more on light therapy alternatives and managing light exposure, see this sun lamp resource.
Doctors may prescribe topical corticosteroids for the affected areas. Systemic corticosteroids are generally avoided except for short-term use to ease symptoms during a severe flare.
Antimalarial drugs may be offered to control symptoms, though these medications tend to be less effective in people who smoke.
Other therapies that might be considered for SCLE include:
Outlook
SCLE cannot be cured, but available treatments can control symptoms and reduce flare-ups. Lifestyle changes also help minimize recurrences.
If a medication is the cause, stopping the drug usually leads to resolution. Symptoms tend to improve within weeks to months after discontinuation.
SCLE lesions rarely produce scarring, although they can leave temporary pigment changes. In most cases, discoloration fades over time.
Since sun avoidance can reduce vitamin D levels, healthcare providers often recommend supplementing with vitamin D and calcium to prevent deficiency.
Talk with your clinician before starting supplements; they can perform blood testing and determine whether supplementation is appropriate for you.
Some individuals with SCLE later develop SLE, meaning internal organs such as the kidneys, lungs, or nervous system could become involved.
Takeaway
SCLE is a form of lupus that primarily affects the skin, causing red, ring-like rashes typically found on the back, arms, torso, or other sun-exposed areas.
Sunlight is a common trigger, so minimizing sun exposure and using protective clothing and sunscreen are important preventive measures.
See a healthcare professional if you notice suspicious rashes and suspect SCLE so you can receive appropriate evaluation and care.























Leave a Reply
You must be logged in to post a comment.