Quick Answer Summary
Some antidepressants can make you feel like you’re stuck on a seesaw—one side lifts your mood, the other flips the night into restless tossing. Others are actually a gentle lullaby, letting you drift off without a prescription for a separate sleep pill. The key is knowing which class, dose, and timing match your personal sleep rhythm. Talk to your prescriber, keep a sleep diary, and remember that a small tweak can turn sleepless nights into refreshed mornings.
Why Sleep Affected
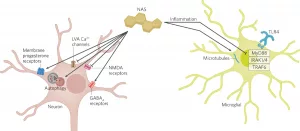
Our brains are wired with chemicals that act like conductors for a symphony of sleep stages. Serotonin, norepinephrine, and histamine each have a part to play. Antidepressants tweak these messengers—sometimes to great effect, sometimes with a few unintended side‑effects.
Neuro‑chemical basics
- Serotonin – low levels can shorten REM sleep; many SSRIs raise serotonin, which can delay sleep onset.
- Norepinephrine – when it spikes, you feel alert; SNRIs often increase it, leading to early‑morning awakenings.
- Histamine – blocks histamine receptors and you get that cozy drowsy feeling; this is why some older antidepressants feel sedating.
What the research says
According to a 2023 network meta‑analysis of antidepressant sleep effects, 13 of the 21 examined drugs increased somnolence, while 11 raised the risk of insomnia. The same study showed that the relationship between dose and sleep side‑effects isn’t always linear—some meds follow an inverted‑U curve, meaning a medium dose may cause more insomnia than a low or high dose.
A 2018 systematic review that pooled 23 randomized trials (2,806 participants) found modest improvements in subjective sleep quality with tricyclic antidepressants (TCAs) like doxepin, but the evidence quality ranged from very low to moderate (see the review). In short, the science is solid enough to give us direction, but still leaves room for personal experience.
Antidepressant Classes
Below is a quick cheat‑sheet that shows which drugs tend to help sleep, which tend to disrupt it, and where the evidence sits.
| Class | Common Drugs | Typical Sleep Effect | Usual Sleep‑Aid Dose |
|---|---|---|---|
| Sedating (Sleep‑Aid) | Doxepin, Mirtazapine, Trazodone, Low‑dose Amitriptyline | ↑ sleep continuity, ↑ total sleep time | Doxepin ≤ 6 mg qHS; Trazodone ≤ 50 mg qHS |
| Activating (Insomnia‑Provoking) | Fluoxetine, Paroxetine, Venlafaxine, Duloxetine, MAOIs | ↑ sleep latency, ↓ REM continuity | — (generally avoid at bedtime) |
| Neutral / Mixed | Bupropion, Vilazodone, Desvenlafaxine | Variable; dose‑dependent | — (monitor individually) |
Sedating antidepressants – the “antidepressant sleep aid”
These drugs are often prescribed off‑label as a sleep aid because they hit the histamine receptors that make you feel cozy. Low‑dose trazodone, for example, is a favorite for people who want a gentle night‑time nudge without the next‑day grogginess that traditional hypnotics sometimes cause.
Activating antidepressants – the “sleep‑disturbers”
If you’re on an SSRI that feels more like a cup of coffee at 10 p.m., you’re not alone. Many patients notice longer time to fall asleep and more early‑morning awakenings. Switching the timing (take it in the morning) or pairing it with a low‑dose sedative can smooth things out.
Choosing the Right
Picking a medication isn’t a lottery; it’s a thoughtful match‑making process.
Clinical decision flow
- Is insomnia the main problem or a side‑effect? If it’s the main issue, a sedating antidepressant may be the single solution.
- Do you need a calming effect at night? Low‑dose doxepin, mirtazapine, or trazodone can double as a sleep aid.
- Are you vulnerable to weight gain or next‑day drowsiness? Avoid high‑dose mirtazapine; consider bupropion, which is weight‑neutral and usually doesn’t affect sleep much.
- Any co‑existing sleep disorder? Restless legs syndrome, sleep apnea, or severe nightmares call for a careful review—some antidepressants can worsen them.
Real‑world example
Meet Maria, a 34‑year‑old graphic designer. She’d been on fluoxetine for six months, but every night felt like a marathon of tossing and turning. After a chat with her psychiatrist, she switched to 3 mg of doxepin taken 30 minutes before bed. Within three weeks, she reported gaining two solid hours of sleep and waking up feeling refreshed. Maria’s story underscores how a tiny dosage adjustment can change the whole night.
Expert insight
Dr. Elena Ruiz, board‑certified sleep psychiatrist, notes, “When depression and insomnia coexist, I first look at the antidepressant’s sleep profile. If the patient can tolerate a low‑dose TCA or a sedating SSRI, it often eliminates the need for a separate hypnotic.” That sentiment aligns with the American Academy of Sleep Medicine’s recommendation to consider a sedating antidepressant as a first‑line option when insomnia is prominent.
Common Side Effects
Even the best‑matched drug can throw a curveball. Below are strategies for the two most common sleep‑related side effects.
When you’re too sleepy
- Adjust timing – move the dose to earlier in the evening or split it into morning and night portions.
- Lower the dose – many sleep‑aid benefits appear at doses far below the antidepressant‑effective range.
- Swap caffeine – a modest cup of coffee after breakfast can counteract lingering drowsiness, but avoid it after 2 p.m.
When you can’t fall asleep
- Consider a switch – moving from an activating SSRI to a low‑dose sedating agent often restores sleep.
- Add CBT‑I – cognitive‑behavioral therapy for insomnia works hand‑in‑hand with medication, improving sleep quality without adding drugs.
- Track and titrate – keep a simple sleep diary for two weeks, noting bedtimes, wake times, and how you feel. Bring it to your appointment; it’s a goldmine for dose adjustments.
Quick‑tips checklist (featured‑snippet ready)
- ✅ Take activating SSRIs in the morning.
- ✅ Use a low‑dose sedating antidepressant 30–60 minutes before bed.
- ✅ Keep a consistent bedtime routine.
- ✅ Review your sleep diary before changing medication.
Beyond Medication
Pharma isn’t the only player in the sleep arena. Pairing medication with evidence‑based non‑drug strategies can boost results dramatically.
Cognitive‑behavioral therapy for insomnia (CBT‑I)
Research shows CBT‑I can rival low‑dose sedating antidepressants in improving total sleep time and sleep efficiency. The approach teaches you to reshape thoughts about sleep, set a regular schedule, and create a bedroom environment optimized for rest.
Sleep‑hygiene hacks
- Dark, cool room – aim for 65 °F (18 °C) and blackout curtains.
- Screen curfew – turn off phones and tablets at least an hour before bed; blue light tricks your brain into staying awake.
- Consistent wake‑time – even on weekends, a regular rise‑time stabilizes your internal clock.
- Relaxation ritual – gentle stretching, reading, or a short meditation can signal to your body that it’s time to wind down.
When to seek professional help
If you notice any of these red flags, it’s time to call your doctor:
- Early‑morning awakenings that leave you exhausted.
- Daytime sleepiness lasting more than two hours.
- Sudden weight gain, nightmares, or worsening mood.
- Any thoughts of self‑harm or a worsening depressive episode.
Final Takeaways
Living with both depression and insomnia can feel like juggling two heavy bags at once. The good news? You don’t have to accept sleepless nights as inevitable. By understanding which antidepressants help or hurt sleep, fine‑tuning dosage and timing, and complementing meds with CBT‑I and solid sleep hygiene, you can reclaim restful nights.
Key points to remember:
- Not all antidepressants are created equal—some are natural sleep aids, others are nocturnal agitators.
- Low‑dose sedating agents (doxepin, trazodone, mirtazapine) often provide the sweet spot of mood improvement plus better sleep.
- Track your sleep, talk openly with your prescriber, and adjust slowly—small changes can have big effects.
What’s your experience with antidepressants and sleep? Have you found a dose or timing that works like a charm? Share your story in the comments or ask your doctor today. Together, we can turn those restless nights into mornings full of possibility.


















Leave a Reply
You must be logged in to post a comment.