Hey there, friend. If you’re scrolling through medical forums, chatting with a doctor, or simply trying to make sense of a recent diagnosis, you’ve probably heard the phrase “immunotherapy before surgery.” It sounds futuristic, right? Turns out it’s already reshaping how we treat several cancers, especially lung cancer. In the next few minutes, let’s unpack what this approach means, why it’s generating excitement, and what you (or a loved one) might expect if you walk down this path. Grab a cup of tea, settle in, and let’s dive in together.
Why Neoadjuvant Matters
First off, “neoadjuvant” is just a fancy medical term for “treatment given before the main surgery.” Think of it like priming a fire—adding kindling (the immunotherapy) before you light the main flame (the operation). The goal? Shrink the tumor, make the surgery easier, and, most importantly, awaken the body’s own immune army to hunt down any hidden cancer cells that might be lurking elsewhere.
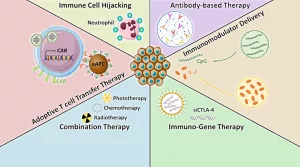
What Exactly Is Immunotherapy Before Surgery?
Immunotherapy refers to drugs that empower your immune system to recognize and destroy cancer cells. The most common classes are PD‑1/PD‑L1 inhibitors (like pembrolizumab or nivolumab) and CTLA‑4 blockers (such as ipilimumab). When these agents are given before the tumor is removed, they can:
- Activate T‑cells while the tumor antigens are still present, essentially giving the immune system a “training session.”
- Reduce tumor size, which can convert an inoperable or borderline case into a clean‑cut surgery.
- Potentially eradicate microscopic disease that imaging can’t see, lowering the chance of recurrence.
Science Behind the Timing
Research indicates that the presence of the tumor provides a rich source of antigens that help “teach” immune cells what to attack. A 2021 review on neoadjuvant immunotherapy highlighted that this “in‑situ vaccination” can lead to lasting immune memory, which may keep cancer at bay long after the scalpel is gone (source).
Clinical Evidence
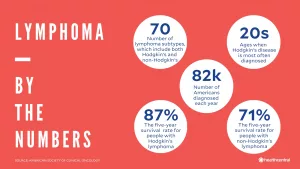
Now, let’s talk real numbers. Across several cancers—most notably non‑small cell lung cancer (NSCLC), melanoma, and even soft‑tissue sarcoma—the data are striking.
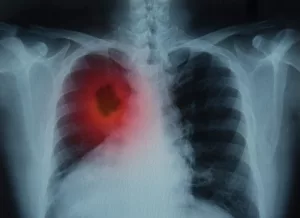
Lung Cancer Takes the Spotlight
NSCLC is the poster child for neoadjuvant immunotherapy. The AEGEAN Phase III trial compared peri‑operative durvalumab plus standard chemotherapy against chemotherapy alone. The results? A 32 % reduction in disease recurrence and a pathologic complete response (pCR) rate of 17.2 % versus just 4.3 % with chemo alone (MD Anderson press release).
Another milestone came from the KEYNOTE‑671 trial, which earned FDA approval for pembrolizumab (Keytruda) both before and after surgery in resectable NSCLC. Early results showed event‑free survival that hadn’t been reached after a median follow‑up of 18 months, meaning patients stayed cancer‑free far longer than historical expectations (Cancer Health article).
And if you wonder how big the benefit really is, a HealthDay summary reported a 42 % lower risk of progression, recurrence, or death when nivolumab was added to pre‑surgical chemotherapy—plus about a quarter of those patients had no detectable cancer after surgery (HealthDay report).
Beyond the Lungs: Melanoma, Sarcoma, Head & Neck
Melanoma fans, listen up: The NADINA trial (stage III melanoma) showed a 27 % drop in death or disease growth and a 68 % reduction in recurrence when nivolumab + ipilimumab were given before surgery (Cancer.org).
Soft‑tissue sarcoma researchers at MD Anderson reported that 90 % of patients treated with a combo of immunotherapy and radiation had less than 15 % viable tumor at surgery, translating into two‑year overall survival rates of 82–90 % (MD Anderson Press).
Even head and neck cancers are feeling the love. A recent study showed that the checkpoint inhibitor bintrafusp alfa, given before resection, boosted the number of exhausted T‑cells that were “re‑invigorated” and spread throughout the bloodstream, potentially warding off future metastases (National Cancer Institute).
Real‑World Benefits
All those percentages look great on a slide, but what does it mean for you?
Tumor Shrinkage Makes Surgery Safer
When the tumor gets smaller, surgeons often need to remove less healthy tissue. This can mean shorter operating times, fewer complications, and quicker recoveries. In a post‑op survey of lung‑cancer patients, many reported less post‑surgical pain and a faster return to daily activities when they’d received neoadjuvant immunotherapy.
Systemic Immune Memory Reduces Recurrence
One of the biggest fears after a “curative” surgery is that hidden cancer cells will sneak back. Immunotherapy before surgery seems to give the immune system a lasting “memory” of those tumor cells, making it easier to spot and destroy any stray cancer cells that try to re‑emerge.
Pathologic Complete Response (pCR) as a Survival Predictor
When pathologists look at the removed tissue and find no viable cancer cells (pCR), it’s a strong predictor of long‑term survival. In the AEGEAN trial, patients achieving pCR were far more likely to remain disease‑free at 2‑year follow‑up.
Potential Risks & Caveats
Good news comes with a pinch of caution. No medical treatment is completely risk‑free, and immunotherapy has its own profile.
Immune‑Related Adverse Events (irAEs)
Because these drugs crank up the immune system, they can sometimes cause the immune system to attack healthy organs—think colitis, dermatitis, pneumonitis, or thyroiditis. Most irAEs are manageable with steroids, and serious events happen in roughly 10‑15 % of patients. Early detection and communication with your oncology team are key.
Surgical Timing & Wound Healing
Studies generally show that checkpoint inhibitors do not delay wound healing, but surgeons often give a short “wash‑out” window (about a week) between the last infusion and the operation to let the immune system settle down.
Who Might Not Benefit?
Patients with very low PD‑L1 expression, active autoimmune disease, or poor organ function may not be ideal candidates. That’s why a thorough pre‑treatment work‑up—including molecular testing and a candid conversation about comorbidities—is essential.
Treatment Journey
| Step | What Happens | Typical Timeline | Patient Touch‑Points |
|---|---|---|---|
| 1️⃣ Molecular Testing | PD‑L1, EGFR, KRAS, and other markers assessed | 1–2 weeks | Pathology report review with oncologist |
| 2️⃣ Neoadjuvant Immunotherapy ± Chemo | 2–4 cycles of checkpoint inhibitor (often with platinum‑based chemo) | 6–12 weeks | Infusion visits, side‑effect monitoring |
| 3️⃣ Restaging Imaging | CT or PET scan to measure tumor response | End of cycle | Radiology review, discussion of surgical plans |
| 4️⃣ Surgery | Lobectomy, pneumonectomy, or tumor‑specific resection | 1–2 weeks after imaging | OR team, post‑op recovery unit |
| 5️⃣ Adjuvant Immunotherapy | Continuation of checkpoint inhibitor for up to 12 months | Post‑operative period | Outpatient clinic visits, labs, imaging follow‑up |
Throughout this journey, you’ll have a multidisciplinary team—medical oncologist, thoracic surgeon, radiologist, and often a nurse navigator—to keep the lines of communication open.
Expert & Patient Voices
Clinician Insight
“Neoadjuvant immunotherapy is a paradigm shift because it lets us watch how a tumor responds in real time,” says Dr. John Heymach, MD, PhD, director of thoracic oncology at MD Anderson. “We can tailor post‑operative therapy based on that response, potentially sparing patients unnecessary toxicity.”
Patient Story
Maria, a 58‑year‑old former teacher diagnosed with stage IIIA NSCLC, recalls the moment her oncologist suggested immunotherapy before surgery. “I was terrified—what if the drugs made things worse?” she admits. After three cycles of nivolumab plus chemo, her scan showed a 55 % shrinkage. “The surgery was smoother than I imagined, and three months later the pathology said ‘no viable cancer.’ That felt like a miracle,” she shares. Maria now follows a survivorship plan that includes regular scans and a supportive‑care group.
Future Directions
More than 30 ongoing trials (e.g., NCT03800134 AEGEAN, NCT03425643 KEYNOTE‑671) are probing the optimal combination, dosing, and biomarkers that predict who will benefit most. The hope is that, within a few years, a simple blood test could tell us whether neoadjuvant immunotherapy is the right move for each individual patient.
Putting It All Together
So, what’s the takeaway?
- Immunotherapy before surgery can shrink tumors, improve surgical outcomes, and teach your immune system to stay on guard.
- For lung cancer, especially resectable NSCLC, the evidence now shows clear survival benefits—sometimes halving the risk of recurrence.
- Side effects exist, but they’re usually manageable with a proactive care team.
- The process involves a series of steps—testing, neoadjuvant treatment, imaging, surgery, and possibly adjuvant therapy—all coordinated by a multidisciplinary team.
If you or a loved one is navigating a cancer diagnosis, consider discussing neoadjuvant immunotherapy as part of your stage III NSCLC treatment options. You might also explore how chemoimmunotherapy for lung cancer fits into your overall plan, learn more about the landscape of non‑small cell lung cancer therapy, or dive deeper into strategies for shrinking lung tumors. Knowledge is power, and the more you understand, the better you can partner with your doctors.
Final Thoughts
Medicine is moving from a “one‑size‑fits‑all” approach to one that’s personalized, dynamic, and—yes—sometimes a little daring. Immunotherapy before surgery exemplifies that evolution. It blends cutting‑edge science with a human touch, giving patients a fighting chance not just to survive, but to thrive.
Remember, you’re not alone on this journey. Whether you’re asking questions in a support group, scrolling through research articles, or sitting across from your oncologist, keep the conversation going. Your curiosity, courage, and collaboration with experts form the best triad for navigating cancer treatment.
Got more questions? Feel free to reach out to your care team, explore reputable resources, or simply share your story with someone who’s walking a similar road. The more we talk, the stronger we all become.



















Leave a Reply
You must be logged in to post a comment.