Hey there. If you’ve landed on this page you’re probably trying to untangle a complex web of medical jargon, appointment schedules, and a flood of emotions that come with a stage III non‑small‑cell lung cancer (NSCLC) diagnosis. Let’s skip the textbook pre‑amble and jump straight into the stuff that matters to you: What can be done, why it matters, and how you can take an active role in the journey ahead. Think of this as a friendly coffee‑chat with someone who’s spent a lot of time listening to patients, reading the latest research, and pulling together the most reliable, easy‑to‑understand information out there.
What Stage Means
Stage III in plain English
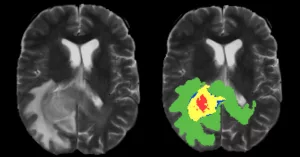
Stage III isn’t a single disease‑state; it’s a family of situations where the tumor has grown beyond the lung itself and has reached nearby lymph nodes. Doctors split it into IIIA (often still surgically removable) and IIIB (usually unresectable). Roughly 30 % of all NSCLC cases are diagnosed at this stage, according to the AZ Early Lung data.
Is it curable?
Good news: for many patients the goal is curative intent, not just palliation. Modern multimodal therapy—think chemotherapy, radiation, and immunotherapy used together—has turned a once‑grim prognosis into a realistic chance of long‑term control. It’s not a guarantee, but it’s a chance worth fighting for.
Common misconceptions
Let’s bust a couple of myths right now. First, “Only surgery can save me.” In reality, more than 80 % of stage III patients have unresectable disease, so surgery is rarely the first weapon. Second, “Immunotherapy alone will cure everything.” Immunotherapy works best when paired with other treatments and when the tumor expresses enough PD‑L1 (usually >1 %). Wrong assumptions can lead to missed opportunities, so ask your team to explain why each therapy is being recommended.
Core Treatment Pillars
1️⃣ Concurrent Chemoradiotherapy (cCRT)
cCRT is the backbone for most unresectable stage III cases. It blends a platinum‑based doublet (often carboplatin plus a second drug) with daily radiation over 6‑7 weeks. The synergy is powerful: chemotherapy sensitizes cancer cells to radiation, and together they shrink the tumor more effectively than either alone.
Who’s a good candidate? Typically patients with a performance status of 0‑1, adequate organ function, and disease that cannot be safely removed by surgery.
Risks to watch include esophagitis (painful swallowing), fatigue, and blood‑count drops that can increase infection risk. Your oncology team will give you a checklist of labs and supportive meds to keep side‑effects in check.
Practical checklist before starting cCRT
| Item | Why it matters |
|---|---|
| Baseline CBC, liver & kidney labs | Detect pre‑existing issues |
| Dental exam & oral hygiene | Prevent severe mouth sores |
| Nutritional assessment | Maintain weight during treatment |
| Medication review | Avoid drug interactions (e.g., NSAIDs) |
Need a deeper dive into the chemo drugs you’ll encounter? Check out our guide on chemoimmunotherapy for lung cancer.
2️⃣ Consolidation Immunotherapy – The Game‑Changer
After cCRT, many patients receive durvalumab (Imfinzi) as a consolidation therapy. The landmark PACIFIC trial showed that adding durvalumab extends overall survival by roughly two years compared with placebo. In plain language: it gives the immune system a “second wind” to mop up any microscopic cancer that survived the chemo‑radiation blitz.
Eligibility – Any unresectable stage III patient who has not progressed after cCRT, regardless of PD‑L1 level (though higher levels may predict a bigger benefit). According to GO2.org, both durvalumab and pembrolizumab are FDA‑approved for this setting.
Safety profile – Immune‑related side‑effects can pop up weeks or months after the first dose. Look out for new cough, shortness of breath, fever, or unexplained fatigue. If you notice anything strange, call your oncology nurse right away. Early intervention usually keeps problems manageable.
Spotting immune‑related side‑effects early
- New or worsening cough – could signal pneumonitis.
- Thyroid changes – weight gain/loss, temperature swings.
- Rash or diarrhea – may indicate colitis or skin toxicity.
Remember, these reactions are generally reversible with steroids or other immunosuppressants if caught early.
3️⃣ Neoadjuvant & Adjuvant Immunotherapy ± Chemotherapy
If your tumor is technically resectable (often stage IIIA with N2 nodal disease), doctors may use a “neoadjuvant” approach—treating before surgery—to shrink the mass and improve surgical outcomes. The FDA has cleared durvalumab combined with chemotherapy as a pre‑op regimen, followed by durvalumab alone after the operation.
Why bother? Studies show higher pathologic complete response rates (meaning no cancer left in the tissue after surgery) and better disease‑free survival. It’s like giving the tumor a double‑hit before you even pick up the scalpel.
Sample timeline for a resectable case
| Week | Intervention | Goal |
|---|---|---|
| 0‑3 | Platinum‑based chemotherapy (2 cycles) | Begin tumor shrinkage |
| 4‑8 | Durvalumab + chemo (neoadjuvant) | Boost immune killing |
| 9‑12 | Surgery | Remove residual disease |
| 13‑24 | Durvalumab (adjuvant) | Prevent recurrence |
Curious about how immunotherapy works before the knife? Read more immunotherapy before surgery.
4️⃣ Targeted Therapy & Molecular Testing
Not every stage III tumor is the same. About 30 % harbor driver mutations (EGFR, ALK, KRAS, MET, etc.). Modern guidelines—see the NCCN 2024 update—recommend comprehensive molecular profiling (tissue plus liquid biopsy) at diagnosis. If a targetable mutation is found, the treatment plan may shift from chemo‑radiation to a precision drug like osimertinib for EGFR‑mutated disease, often combined with localized radiation.
This isn’t just academic; it can spare you from the harshness of chemotherapy and give you a more tolerable, effective option.
Quick FAQ on testing
- Do I need a liquid biopsy? Yes. It catches mutations that a tissue sample might miss.
- How long does it take? Usually 7‑10 days.
- Will insurance cover it? In most markets, yes—especially when ordered by an oncologist.
For a fuller look at the landscape of non‑small cell lung cancer therapy, check out our dedicated article.
Balancing Benefits & Risks
Every treatment brings a trade‑off. Below is a simple matrix to help you and your team weigh the upside against the possible downside.
| Benefit | Risk / Side‑Effect |
|---|---|
| Improved overall survival (up to 55 % 3‑year OS with cCRT + durvalumab) | Immune‑related pneumonitis, thyroiditis, skin rash |
| Higher chance of complete tumor removal (neoadjuvant therapy) | Surgical delay if severe toxicity occurs |
| Targeted therapy avoids chemo toxicity in mutation‑positive patients | Potential for resistance mutations over time |
| Symptom relief (shrinking lung tumors reduces cough, shortness of breath) | Fatigue, nausea, appetite loss |
The key is shared decision‑making. Ask your doctor to explain the numbers in a way that makes sense for your lifestyle, age, and personal goals. Remember, “quality of life” is as important as “quantity of life.”
Real‑World Stories
Case 1 – The “Triple‑Combo” Success
Mike, 58, was diagnosed with stage IIIA disease that was technically resectable. He received neoadjuvant chemotherapy plus durvalumab, underwent a lobectomy, and continued durvalumab for a year. Pathology showed no residual cancer—a complete response. Two years later, he’s still disease‑free and back to hiking his favorite trails.
Case 2 – The Unresectable Warrior
Laura, 66, had stage IIIB disease that couldn’t be removed surgically. She completed cCRT, then switched to durvalumab maintenance. While she experienced mild fatigue and a brief episode of thyroiditis, the side‑effects were manageable. Today, she reports a better quality of life than she expected and continues to enjoy gardening.
Case 3 – The Targeted‑Therapy Turnaround
Samuel, 72, was found to have an EGFR exon‑19 deletion. Instead of the standard chemo‑radiation, his team started osimertinib with focused radiation to a troublesome lymph node. Six months later, scans show a >70 % reduction in tumor size, and his cough has nearly vanished—talk about “shrinking lung tumors”!
Do any of these stories echo your own experience? If you’ve walked a similar path, sharing your journey can empower others. Feel free to reach out to our community forum (link in the sidebar) to exchange tips and encouragement.
Your Next Steps
How to talk to your care team
1. Bring a medication list. Include over‑the‑counter pills and supplements—they can interact with chemo or immunotherapy.
2. Gather your imaging and pathology reports. Having them on hand speeds up discussions.
3. Ask about clinical trials. Many phase II/III studies accept stage III patients, offering access to cutting‑edge treatments.
4. Request a written treatment timeline. Seeing the plan on paper helps you track progress and anticipate appointments.
Take action today
If you haven’t already, schedule a multidisciplinary tumor‑board meeting. This gathering of a thoracic surgeon, radiation oncologist, medical oncologist, pulmonologist, and a nurse navigator ensures every angle is considered. Ask them to explain why each component (cCRT, immunotherapy, targeted therapy) is recommended for you specifically.
And remember, you’re not alone. Leverage resources like patient‑advocacy groups, counseling services, and the links we’ve sprinkled throughout this article. Empowerment starts with knowledge, and knowledge becomes power when you turn it into action.
Bottom Line
Stage III NSCLC treatment is a dynamic, multimodal journey that blends chemotherapy, radiation, immunotherapy, and—when appropriate—targeted drugs. The goals are clear: shrink the tumor, eliminate microscopic disease, and give you a realistic chance at long‑term control. By staying informed, asking the right questions, and partnering with a dedicated multidisciplinary team, you can navigate this complex landscape with confidence.
Ready to learn more? Dive into our guide on shrinking lung tumors, or explore specific therapy options in our non‑small cell lung cancer therapy hub. Your health story is still being written—let’s make the next chapter hopeful and strong.






















Leave a Reply
You must be logged in to post a comment.