Hey there, friend. If you’ve just heard that your doctor mentioned “shrinking lung tumors,” you’re probably feeling a mix of hope, anxiety, and a flood of questions. What does it actually mean? How fast can you expect a tumor to get smaller? Which treatments give the best chance of a noticeable reduction? Let’s sit down together (virtually, of course) and walk through the answers, step by step. I’ll keep the medical jargon to a minimum, sprinkle in some real‑world stories, and—most importantly—make sure you leave feeling more informed and a little less alone.
Why Shrink Tumors
First, why do we focus on tumor shrinkage in the first place? Think of a stubborn knot in a rope. If you can pull it loose, the rest of the rope becomes easier to handle. When a lung tumor gets smaller, many things improve:
| Benefit | Possible Risk |
|---|---|
| Makes surgery or curative resection possible | Tumor may regrow (progression) |
| Relieves symptoms like coughing, shortness of breath | Side‑effects from systemic therapy (fatigue, nausea, immune‑related reactions) |
| Helps doctors stage the disease more accurately | Misinterpreting “pseudo‑progression” as growth |
Balancing these benefits and risks is the heart of every treatment conversation. Your care team will weigh how likely a therapy is to shrink the tumor against how tolerable its side‑effects are for you.
Top Treatment Options
Chemo‑Immunotherapy
This combo pairs a platinum‑based chemotherapy with an immune checkpoint inhibitor such as pembrolizumab or atezolizumab. In a 2022 review, chemo‑immunotherapy achieved a 48 % objective response rate in unresectable non‑small cell lung cancer (NSCLC) according to a major NEJM study. Most patients see measurable shrinkage after the first two cycles—roughly four to six weeks.
Curious how this feels in real life? One patient shared on an online forum that their tumor “halved after just three weeks on osimertinib,” a targeted drug, but many also report similar rapid drops with chemo‑immunotherapy. The synergy works because chemotherapy weakens the cancer cells while immunotherapy awakens your own immune army to finish the job.
Looking for more depth on this approach? Check out our guide on chemo‑immunotherapy for lung cancer.
Targeted Therapy
If your tumor carries a specific genetic “driver”—like EGFR, ALK, or ROS1—targeted pills can be a game‑changer. These drugs lock onto the mutated protein and shut it down, often shrinking the tumor within two weeks. A patient in the Inspire community wrote, “My dad’s EGFR‑mutated tumor halved after 3 weeks on osimertinib.” The median time to best response sits around eight weeks, but the early dip is encouraging.
Radiation‑Based Approaches
Stereotactic Body Radiotherapy (SBRT)
SBRT delivers high‑precision, high‑dose radiation in a handful of sessions. A 2020 study by Vu et al. showed that patients who achieved ≥30 % tumor‑volume shrinkage during SBRT enjoyed markedly better disease‑free survival (see the Journal of Radiation Research).
Typically, you’ll notice a size reduction after the third or fourth fraction, with the most dramatic change by three months post‑treatment.
Shrinking‑Field Radiation for Stage III
For locally advanced stage III NSCLC, doctors sometimes start with a larger radiation field and then “shrink” it as the tumor responds. This tactic preserves healthy tissue while still delivering a curative dose. It also sets the stage for possible surgery later on—something we’ll explore under stage III NSCLC treatment.
Local Ablation Techniques
When surgery isn’t an option, minimally invasive ablation can physically destroy tumor cells:
- Radiofrequency ablation—a thin probe heats the tumor from the inside, often achieving up to 80 % reduction of the targeted nodule.
- Photodynamic therapy—a light‑activated drug and laser combination, ideal for airway‑blocking lesions.
- Cryotherapy—extreme cold freezes cancer cells, improving breathing in patients with airway obstruction.
All these procedures aim to shrink the tumor enough to relieve symptoms and, in some cases, make future surgery feasible.
How Fast Shrinkage
Speed varies by treatment modality, tumor biology, and individual health. Here’s a quick snapshot:
| Modality | Median Time to Detectable Shrinkage | Typical % Reduction (first scan) |
|---|---|---|
| Chemo‑immunotherapy | 4–6 weeks | 30–45 % |
| Targeted therapy (EGFR, ALK) | 2 weeks | 35–50 % |
| SBRT | 3 weeks post‑treatment | 40–60 % (by 3 months) |
| Radiofrequency ablation | Within 48 hours | Up to 80 % |
| Photodynamic therapy | 1–2 weeks | 20–35 % |
In practice, most oncologists schedule a “mid‑treatment” scan after 2–3 cycles of systemic therapy and a “post‑treatment” scan 8–12 weeks after the final dose. This timing aligns with NCCN’s 2024 recommendations for NSCLC restaging according to NCCN.
Factors Influencing Shrinkage
Not every tumor responds the same way. Several variables shape the outcome:
- Histology & stage—Small‑cell lung cancer often shrinks quickly with chemo, while advanced‑stage NSCLC may need multimodal therapy.
- Molecular profile—Presence of EGFR, ALK, KRAS, or high PD‑L1 can tip the scales toward targeted or immunotherapy success.
- Patient’s performance status—Better overall health usually translates to stronger treatment tolerance and, subsequently, better shrinkage.
- Treatment adherence—Missing cycles can blunt the response.
- Imaging technique—Volumetric CT measurement (instead of simple RECIST 1.1) can detect subtle changes earlier.
When you talk with your care team, ask about each of these factors. Understanding your tumor’s unique fingerprint helps set realistic expectations.
Real Patient Stories
Numbers are reassuring, but real people bring the data to life. Here are three snippets pulled from supportive‑care forums (all shared voluntarily):
- 2013, Inspire “Tumor Shrinking!!” – A patient reported steady tumor reduction after each chemo cycle, noting that “shrinkage is good but may plateau.”
- 2020, Inspire “Lung nodule shrink?” – A 39‑year‑old’s suspicious nodule halved in three weeks after antibiotics treated an infection, illustrating that not every shrinkage signals cancer.
- 2024, Inspire “Tumor shrinking!” – A husband on Alimta + Keytruda saw his tumor drop from 3.2 cm to 1.7 cm. The family wondered whether chemo or immunotherapy was driving the change—an exact question many of us ask.
These anecdotes underline a key point: tumor shrinkage can result from treatment, infection resolution, or even natural fluctuation. Always confirm with your oncologist before drawing conclusions.
How To Monitor Progress
Monitoring is the compass that tells you whether you’re on the right path. Here’s a practical roadmap:
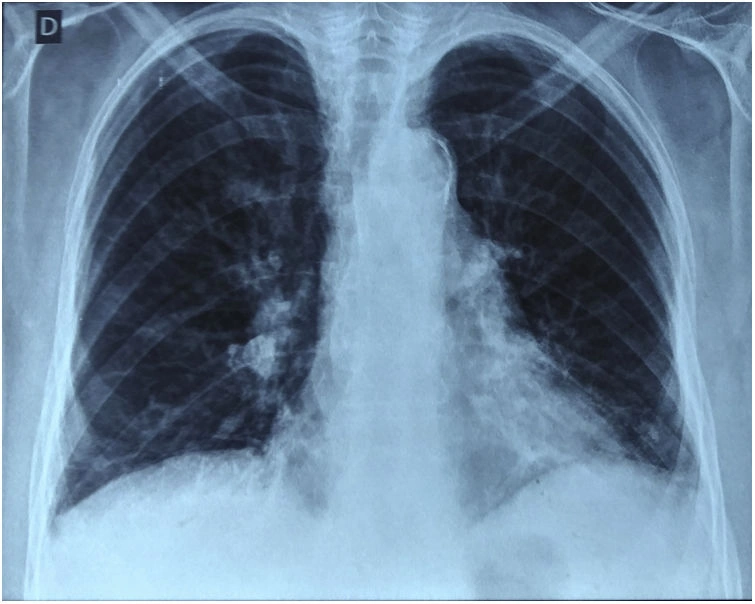
- Baseline imaging – A high‑resolution CT (often paired with PET) before any therapy.
- Mid‑treatment check – Usually after 2–3 cycles of chemo‑immunotherapy or halfway through SBRT. This helps gauge early response.
- Post‑treatment scan – 8–12 weeks after finishing the regimen, per NCCN guidelines.
- Symptom diary – Track cough, breathlessness, fatigue, and any new pains. Sudden changes merit a prompt call to your team.
- Red‑flag alerts – New lesions, increasing SUV on PET, or rapid symptom worsening should trigger early re‑evaluation.
Think of this schedule as your personal health GPS. If you ever feel “lost,” a quick chat with your nurse navigator can re‑align the route.
Bottom Line Advice
Shrinking a lung tumor is more than a hopeful phrase—it’s a concrete, achievable goal in modern oncology. Whether you’re leaning on chemo‑immunotherapy, targeted pills, precise radiation, or a combination of local ablative tricks, evidence shows that many patients see significant tumor reduction within weeks to a few months.
The journey is rarely linear. Tumors can pause, bounce back, or even “pseudo‑progress,” where scans look worse before they get better. That’s why regular imaging, open communication with your multidisciplinary team, and a clear understanding of the benefits versus risks are essential.
Remember, you’re not navigating this alone. Your doctors, nurses, support groups, and even strangers sharing their stories online are all part of a larger community rooting for you. Keep asking questions, note every change—no matter how small—and celebrate every inch of shrinkage, because each one is a step toward better breathing, better treatment options, and ultimately, a better quality of life.
If you want to dive deeper into specific treatment pathways, explore our detailed guides on non‑small cell lung cancer therapy, immunotherapy before surgery, and the comprehensive stage III NSCLC treatment. Knowledge is power, and together we can turn that power into hope.




















Leave a Reply
You must be logged in to post a comment.