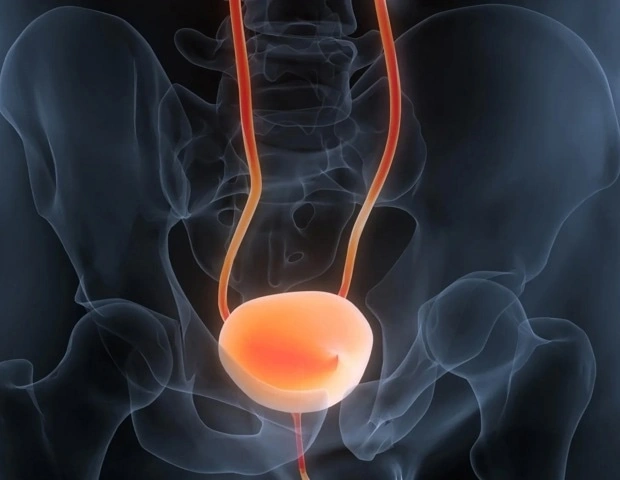
Most people don’t realize that a simple urine test can flag the risk of bladder cancer coming back before a scan even shows it. Below you’ll learn what the test is, why it matters after immunotherapy, and what you can do today to lower your odds of another tumor.
Imagine you’ve just finished a tough round of bladder cancer treatment. You’re relieved, but a lingering “what‑if” keeps nudging at the back of your mind. That feeling is normal—and it’s exactly why understanding bladder cancer recurrence is so vital. Let’s dive in together, step by step, and turn uncertainty into confidence.
What Is Recurrence
In plain language, recurrence means the cancer cells have decided to make a comeback after you’ve had them treated. It can happen in the bladder’s lining, the surrounding pelvic area, or even far‑off places like the liver or bones.
According to a 2013 UCLA study, nearly three‑quarters of patients with high‑grade non‑muscle‑invasive bladder cancer see the disease return within ten years. That sounds scary, but the good news is that early detection and personalized care can dramatically cut that risk.
Where Does It Return
| Site | Typical % of Recurrences | Average Time to Return |
|---|---|---|
| Pelvic lymph nodes | 55 % | 13–22 months |
| Retro‑peritoneal nodes | 33 % | 12–18 months |
| Local bladder wall | 45 % | 6–14 months |
| Distant (liver, bone, lung) | ≈ 30 % | Varies |
These numbers come from a 2003 imaging study that examined 42 patients after radical cystectomy. Pelvic lymphadenopathy was the most common pattern, highlighting why vigilant follow‑up is essential.
Why Some Risks Can Be Managed
Not everything is out of your hands. While age, tumor stage, and genetics are fixed, you can influence treatment compliance, lifestyle choices, and the frequency of surveillance. A 2024 analysis of Medicare data showed that patients who adhered to recommended intravesical therapy (like BCG or chemotherapy washes) had a 30 % lower chance of recurrence.
utDNA Overview
Enter urine‑based tumor DNA (utDNA)—the breakthrough many clinicians call a “liquid biopsy for the bladder.” Tiny fragments of cancer DNA float in your urine after a tumor sheds cells. The test looks for specific mutations and methylation patterns that are unique to bladder cancer.
In a multi‑institutional study published on Science Direct, researchers found that utDNA could predict which patients would relapse after checkpoint‑inhibitor immunotherapy with about 85 % sensitivity and 80 % specificity. In plain English: it’s a pretty reliable early warning system.
How the Test Works
1. Sample collection – You provide a first‑morning urine sample, ideally before any bladder‑instillation therapy.
2. DNA extraction – Lab technicians isolate cell‑free DNA from the fluid.
3. Sequencing & analysis – Advanced algorithms compare the fragments to a library of known bladder‑cancer mutations.
4. Result report – You receive a risk score (low, intermediate, or high) that your doctor can act on.
If you want a deeper dive into the science, check out our utDNA testing page.
When to Get Tested
Timing matters. Most experts recommend the first test 4–6 weeks after the last dose of immunotherapy or intravesical chemotherapy, then every 3–6 months for the first two years. The early period is crucial because the majority of recurrences happen within the first 24 months.
Traditional Surveillance
For decades, the gold standard has been cystoscopy, imaging (CT or MRI), and urine cytology. While cystoscopy gives a direct visual, it’s invasive and can miss flat lesions. Adding utDNA to the mix lets you catch molecular changes before they become visible.
Imagine you’re scheduled for a cystoscopy in six months. Your doctor orders an utDNA test today, and the result comes back “high risk.” Instead of waiting, you get a targeted cystoscopy now, discover a tiny lesion, and treat it before it grows. That’s the power of combining old and new.
Personalized Cancer Therapy
Once you know your utDNA risk score, you can tailor personalized cancer therapy:
- Low risk – Extend cystoscopy interval, continue routine intravesical maintenance.
- Intermediate risk – Add a second intravesical agent (e.g., gemcitabine) or a short course of systemic chemo.
- High risk – Consider early systemic immunotherapy, clinical trial enrollment, or intensified imaging.
These choices aren’t “one‑size‑fits‑all.” Your oncologist will weigh the tumor’s grade, prior treatments, and your personal health goals. The key is that utDNA gives you a data‑driven conversation starter.
Real‑World Example
Meet Mark, a 62‑year‑old former smoker who completed six BCG installations after a stage Ta tumor. His last cystoscopy was clean, but his utDNA test returned a high‑risk score three months later. The physician performed an early TURBT (transurethral resection of bladder tumor) and found a tiny carcinoma in situ that would have been missed on the standard schedule. After a brief course of intravesical gemcitabine, his utDNA score dropped to low, and he’s now three years recurrence‑free.
Mark’s story shows how a simple urine sample can save you from an extra surgery—or at least give you a head start.
Risks & Limitations
Nothing is perfect. False‑positives can cause anxiety and lead to unnecessary procedures, while false‑negatives might give a false sense of security. Technical factors—like improper sample handling—can affect accuracy. That’s why most guidelines recommend confirming a positive utDNA result with cystoscopy.
Access can also be uneven. Some community hospitals haven’t yet adopted the test, and insurance coverage varies. It’s worth checking with your provider; many plans reimburse when a board‑certified urologist orders the test.
Practical Steps for You Today
- Ask your urologist about utDNA testing after your recent immunotherapy or BCG course.
- Schedule a baseline cystoscopy if you haven’t had one in the past three months.
- Track symptoms—blood in urine, new pain, changes in frequency.
- Follow a surveillance calendar—we’ve created a printable version you can download (just search “bladder cancer recurrence calendar”).
- Adopt supportive habits—quit smoking, stay hydrated, eat antioxidant‑rich foods, and keep active.
Every step you take is a stitch in the safety net that keeps recurrence at bay.
Key Takeaways
• bladder cancer recurrence is common, especially within the first two years.
• utDNA is a non‑invasive, highly predictive test that can guide earlier intervention.
• Pair utDNA with traditional cystoscopy for the most complete picture.
• Personalized therapy—adjusting intravesical, systemic, or surgical options based on risk—offers the best chance to stay recurrence‑free.
• Lifestyle choices and treatment compliance are powerful tools you control.
Remember, you’re not alone on this journey. The science is evolving, but the heart of the matter is simple: stay informed, stay proactive, and lean on the experts (and your supportive friends). If you have questions, reach out to your care team—they’re there to help you navigate each step.
What’s the next move you’ll make for your health? Share your thoughts or any experiences you’d like to discuss. Together we can turn uncertainty into confidence and keep the future bright.




















Leave a Reply
You must be logged in to post a comment.