Imagine your brain as a bustling city that never sleeps. Every thought, memory, and movement needs power—tiny bursts of energy delivered exactly where and when they’re needed. That power comes from neuron metabolism, the set of biochemical pathways that turn food, sugars, and even fat into the ATP that keeps neurons firing. In the next few minutes we’ll walk through what fuels those cells, how the energy‑budget stays balanced, what goes wrong in rare epilepsies, and what you can do if you suspect a metabolic problem. Grab a coffee, settle in, and let’s chat about the brain’s hidden energy secrets.
Fuel Sources for Neurons
What fuels a neuron?
Neurons love glucose. It slides into the cell via GLUT3 transporters, runs through glycolysis, and the resulting pyruvate enters the mitochondria for the full oxidative‑phosphorylation cascade. But glucose isn’t the whole story. Astrocytes—a type of star‑shaped glial cell—grab glucose from the blood, convert it to lactate, and hand the lactate off to neurons through monocarboxylate transporters (MCT1/2). This “astrocyte‑neuron lactate shuttle” is like a friendly neighborhood delivery service, keeping neurons supplied when they’re firing fast.
Can neurons use fat?
For a long time, fat was thought to be off‑limits for the brain. Recent work, however, showed that neurons can store tiny droplets of triglycerides and tap into them during prolonged activity. A 2019 Frontiers study reported that lipid droplets act as a short‑term reserve, especially when glucose is scarce.
Why is the energy budget per neuron “fixed”?
Surprisingly, a cortical neuron in a mouse consumes about the same amount of ATP as one in a human—roughly 10⁹ ATP molecules per second. This “fixed energy per neuron” principle was highlighted in a 2011 scaling analysis, which showed that brain size grows by adding more neurons rather than by making each neuron more power‑hungry. According to that study, the brain’s total energy use scales linearly with neuron count.
Astrocyte‑neuron partnership
Astrocytes do more than hand over lactate. Their end‑feet hug capillaries, mop up excess potassium, clear glutamate, and buffer pH—all tasks that cost energy. By keeping the extracellular environment tidy, astrocytes spare neurons from having to run their own “cleanup crew.” In short, think of astrocytes as the supportive friends who bring snacks, clean the table, and make sure the party (your synaptic signaling) never runs out of juice.
Key metabolic players
| Category | Protein / Enzyme | Primary Role |
|---|---|---|
| Glucose Transport | GLUT1 (BBB), GLUT3 (neurons) | Import glucose from blood |
| Lactate Shuttle | MCT1 (astrocytes), MCT2 (neurons) | Move lactate between cells |
| Citrate Transport | SLC13A5 (Na⁺‑coupled citrate transporter) | Export citrate for TCA cycle |
| Na⁺/K⁺‑ATPase | α‑subunit isoforms | Maintain ion gradients, huge ATP consumer |
| Fatty‑Acid Oxidation | CPT1, ACADs | Burn lipid droplets when needed |
Mitochondrial Regulation Basics
How do mitochondria get to the right spot?
Mitochondria travel along microtubules using motor proteins—kinesin for anterograde (toward the synapse) and dynein for retrograde (back to the soma). When a neuron fires, calcium spikes signal nearby mitochondria to pause, dock, and start producing ATP right where it’s needed. Think of them as tiny power plants that park themselves at the busiest intersections.
What happens when transport fails?
If the “high‑way” for mitochondria breaks down, energy deserts appear at synapses. This can happen with a faulty transport protein: a mutation that disrupts motor‑protein binding or microtubule stability. The result? Synaptic fatigue, reduced plasticity, and in severe cases, neurodevelopmental disorders.
Clinical clue: SLC13A5 epilepsy
Mutations in the SLC13A5 gene cripple the sodium‑coupled citrate transporter, a brain transport protein that shuttles citrate out of neurons for the TCA cycle. Without enough citrate, the metabolic engine sputters, leading to early‑onset seizures and developmental delay. For a deeper dive, see the SLC13A5 epilepsy page.
Practical tip for researchers
Live‑cell imaging with JC‑1 dye lets you watch mitochondrial membrane potential in real time. Pair that with calcium imaging, and you can correlate energy supply with firing rates—exactly the kind of data that moves the field forward.
When Metabolism Breaks Down
SLC13A5 epilepsy explained
The SLC13A5 transporter normally moves citrate from the mitochondrial matrix into the cytosol, where it fuels fatty‑acid synthesis and regulates neuronal excitability. When the gene is mutated, citrate stays locked inside mitochondria, the TCA cycle slows, and neurons become hyper‑excitable. The clinical picture often includes generalized seizures within the first weeks of life, sometimes accompanied by developmental regression.
Faulty transport proteins in other disorders
Consider GLUT1 deficiency syndrome, where a faulty transport protein blocks glucose entry across the blood‑brain barrier. Children present with seizures, ataxia, and microcephaly—classic signs that the brain is starving for fuel. Treatment with a ketogenic diet (which supplies ketone bodies that bypass the GLUT1 block) can dramatically improve outcomes.
Severe epileptic encephalopathy and energy
In severe epileptic encephalopathy, continual high‑frequency firing exhausts ATP stores, overwhelms mitochondrial buffering, and triggers a cascade of oxidative stress. The vicious cycle can be broken by early metabolic interventions—ketogenic diets, mitochondrial cofactors (CoQ10, nicotinamide riboside), and, when applicable, gene‑targeted therapies.
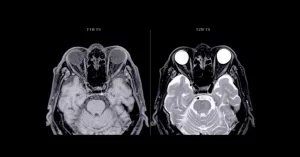
Neurodegeneration links
Chronic hypometabolism is a hallmark of Alzheimer’s and Parkinson’s disease. FDG‑PET scans consistently show reduced glucose uptake in affected regions. The underlying cause may be mitochondrial dysfunction, impaired glucose transport, or a combination of both. By bolstering neuronal energy—through diet, exercise, or targeted drugs—we may slow disease progression.
Therapeutic angles
- Ketogenic diet: Provides ketone bodies that enter the TCA cycle without needing glucose transport.
- Gene therapy: Early trials aim to replace defective SLC13A5 or GLUT1 genes.
- Mitochondrial boosters: Coenzyme Q10, riboflavin, and NAD⁺ precursors have shown modest benefits in animal models.
- Precision nutrition: Tailoring carbohydrate, fat, and protein ratios based on individual metabolic profiling.
Measuring Brain Energy
Imaging the hungry brain
FDG‑PET (fluorodeoxyglucose positron emission tomography) visualizes glucose uptake across the whole brain, highlighting hypometabolic hotspots. For finer detail, ¹³C‑magnetic‑resonance spectroscopy (MRS) tracks labeled glucose as it travels through metabolic pathways. A 2017 review in Frontiers explained how ¹³C‑MRS can differentiate neuronal versus astrocytic oxidation rates.
Biomarkers you can order
- CSF lactate/pyruvate ratio – high ratio suggests mitochondrial dysfunction.
- Blood ketone bodies – useful in monitoring ketogenic diet compliance.
- Plasma citrate levels – low levels may hint at SLC13A5 deficiency.
Scaling data across species
When reading animal studies, remember the “fixed energy per neuron” rule. A mouse brain and a human brain may differ in size, but each neuron’s ATP demand is roughly the same. This helps translate findings from rodents to the clinic.
Checklist for Care
Screening & Diagnosis
- Take a detailed seizure history (onset age, triggers, response to diet).
- Order a basic metabolic panel: glucose, lactate, ketones.
- Consider genetic testing for GLUT1, SLC13A5, and other transport proteins if seizures are refractory.
- If metabolic suspicion persists, schedule FDG‑PET or ¹³C‑MRS.
Management Strategies
- Implement a ketogenic or low‑glycemic diet under dietitian supervision.
- Start mitochondrial support supplements (CoQ10 100 mg bid, nicotinamide riboside 250 mg daily).
- Monitor growth, developmental milestones, and seizure frequency closely.
- Stay in touch with a multidisciplinary team: neurologist, metabolic specialist, and genetic counselor.
When to seek help
If you notice any of the following, reach out to your healthcare provider promptly:
- New or worsening seizures despite medication.
- Developmental regression or loss of previously acquired skills.
- Unexplained fatigue, headaches, or difficulty concentrating.
- Family history of rare metabolic epilepsy.
Wrapping It All Up
Neuron metabolism is the invisible engine that powers every thought you have, every song you hum, and every step you take. By understanding the fuel sources, the tight mitochondrial choreography, and the ways the system can go awry, we empower ourselves—and our loved ones—to catch problems early and act wisely. Whether you’re a clinician, a researcher, or a curious reader, the take‑home message is simple: the brain loves balance, and a little attention to its energy needs can make a world of difference.
What’s your experience with brain‑fuel topics? Have you tried a ketogenic diet, or do you know someone navigating a rare metabolic epilepsy? I’d love to hear your story—feel free to share in the comments below. And if any of the information sparked a question, don’t hesitate to ask. Together, we can keep our brains humming along smoothly.


















Leave a Reply
You must be logged in to post a comment.