Imagine swapping out dozens of daily insulin shots for a tiny, living “mini‑organ” that talks to your body the way nature intended. That’s the promise of functional human islets – clusters of insulin‑producing cells grown in the lab that behave like the real thing. In the next few minutes I’ll walk you through what these islets are, how scientists coax them out of stem cells, why they matter for type 1 diabetes treatment, and what hurdles still lie ahead. Grab a coffee, settle in, and let’s explore this exciting frontier together.
Quick Primer
What does “functional” really mean?
When researchers call an islet “functional” they mean it can sense glucose levels and release the right amount of insulin – just like a healthy pancreas. In the lab this is measured with glucose‑stimulated insulin secretion (GSIS) assays, calcium‑flux imaging, and viability tests. A functional islet should respond within minutes to a rise in blood glucose and shut off when sugars drop, mimicking the physiological rhythm we rely on every day.
How are they different from native pancreatic islets?
Native islets live in a perfectly wired 3‑D architecture, surrounded by blood vessels and nerves. Lab‑grown islets (often called SC‑islets or HILOs) aim to recapitulate that micro‑organ, but they start from pluripotent stem cells instead of embryonic tissue. Studies show that while SC‑islets match native islets in insulin content, they sometimes lack the fully mature beta‑cell signature or the intricate vascular network that native tissue enjoys (a study).
Science Behind Creation
Step‑by‑step of the 7‑stage protocol
Think of the 7‑stage protocol as a culinary recipe for islet making:
- Stage 1 – Definitive endoderm induction: Small molecules push stem cells toward gut‑lineage.
- Stage 2 – Primitive gut tube formation: Growth factors like FGF10 shape the tube.
- Stage 3 – Posterior foregut patterning: Retinoic acid nudges cells toward the pancreas.
- Stage 4 – Pancreatic progenitor specification: Activin‑A and Noggin encourage PDX1 expression.
- Stage 5 – Endocrine lineage commitment: NEUROG3 turns on the beta‑cell program.
- Stage 6 – Beta‑cell maturation: Nicotinamide and thyroid hormone refine insulin production.
- Stage 7 – Aggregate formation: Cells self‑assemble into 3‑D clusters that look and act like islets.
The magic happens in the last stage, where cells are encouraged to form spheroids either in microwells or rotating bioreactors.
3D culture options: Microwells vs. rotating suspension
Two popular methods shape the final islet size and uniformity:
- Microwells: Tiny, defined wells produce homogeneous aggregates (≈100 µm). Researchers report higher success rates and less clumping.
- Rotating suspension: Cells float freely, leading to a mix of sizes; some aggregates grow large and sometimes fuse, which can impair nutrient diffusion.
In a 2022 comparison, microwell‑derived aggregates showed a 30 % increase in insulin secretion consistency compared with rotating‑suspension cultures (a study).
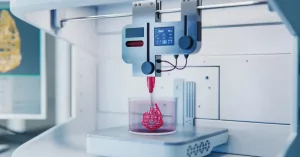
Emerging technologies: 3D bioprinting and bioink
Imagine printing a tiny organ layer by layer, just like a 3‑D‑printed coffee mug. That’s the idea behind 3D bioprinting islets. Researchers embed stem‑derived beta cells in a supportive “bioink” – a gelatinous matrix that mimics the extracellular environment. Once printed, the structure solidifies, and the cells begin to self‑organize into a functional islet.
If you’re curious about the materials that make this possible, check out our guide on bioink for diabetes. The combination of precise architecture and a nurturing matrix could solve the lingering problem of poor vascularization in lab‑grown islets.
Pre‑clinical Evidence
In‑vitro glucose‑stimulated insulin secretion (GSIS)
Lab tests show that mature SC‑islets release roughly 2‑3 µU insulin per islet in response to high glucose – comparable to cadaveric human islets. Calcium‑imaging further confirms that beta cells fire calcium spikes when glucose spikes, a hallmark of functional maturity.
In‑vivo transplantation outcomes
When researchers transplanted stage‑7 aggregates under the kidney capsule of immunodeficient mice, the grafts quickly became glucose‑responsive. Mice that had received a modest dose (≈250 islet equivalents) maintained normal blood glucose for weeks, even after a streptozotocin challenge that normally induces severe hyperglycemia.
Case study: Mouse model of streptozotocin‑induced diabetes
One group of mice received 300 SC‑islets; another group received the same number of native human islets. Both cohorts restored normoglycemia within 48 hours, but the SC‑islet group showed slightly slower insulin peak times, suggesting room for maturation improvement.
Immunoprotection strategies
Because the immune system is the biggest roadblock for any cell‑based therapy, scientists have explored two main tactics:
- Encapsulation: Islets are sealed in a semi‑permeable alginate capsule that lets glucose and insulin pass but blocks immune cells.
- Gene editing: CRISPR is used to knock out HLA‑A/B antigens, rendering the cells less visible to T‑cells.
Recent work even demonstrated “HILOs” (human islet‑like organoids) that can evade immune attack without an external shield, a breakthrough that could simplify regulatory pathways (according to a review).
Clinical Translation: What It Means for Type 1 Diabetes
Current landscape of type 1 diabetes treatment
Today, most patients rely on rapid‑acting insulin injections or pumps. While tech advances like continuous glucose monitors have improved day‑to‑day control, none restore the body’s natural insulin pulsatility. A functional human islet graft could theoretically provide that missing physiological feedback loop, reducing hypoglycemia risk and the burden of daily dosing.
Potential benefits of functional human islets
- Physiologic insulin release: Real‑time response to meals, exercise, stress.
- Reduced injection burden: One transplant could replace dozens of daily shots.
- Improved quality of life: More freedom, fewer “blood‑sugar rollercoasters.”
Risks & challenges
It’s not all sunshine. Here are a few realistic concerns:
- Immune rejection: Even with encapsulation, the body may form fibrotic overgrowth.
- Scalability: Producing enough islets for a human (≈1 million islet equivalents) remains a manufacturing hurdle.
- Regulatory pathway: Cell‑based products must meet stringent FDA criteria for safety, purity, and consistency.
Safety data from recent animal studies
In a 2023 mouse study, transplanted SC‑islets remained viable for over 100 days without tumor formation. Vascular integration was observed via CD31 staining, suggesting that the graft can attract its own blood supply, a key step toward long‑term function.
Regulatory and manufacturing roadmap
To move from bench to bedside, labs must adopt Good Manufacturing Practice (GMP)‑compatible bioreactors, validate each differentiation step, and perform rigorous release testing (purity, potency, sterility). The FDA has issued a “fast‑track” designation for cell‑based diabetes therapies, but developers still need phase‑I safety data before larger trials can begin.
Future Directions & Real‑World Applications
3D bioprinting islets – from prototype to bedside
Researchers have already printed 3D printed islets using a bioink that contains extracellular matrix proteins and micro‑vascular channels. The printed structures showed improved oxygen diffusion, a common bottleneck for large aggregates. As the technology matures, we might see custom‑shaped islet patches tailored to a patient’s anatomy.
Combining functional islets with bio‑ink scaffolds
One promising approach merges the best of both worlds: embed SC‑islets in a hydrogel that mimics pancreatic stroma, then print them into a lattice that encourages blood vessel ingrowth. Below is a quick comparison of two popular encapsulation strategies.
| Feature | Alginate Encapsulation | Bio‑ink Scaffold |
|---|---|---|
| Porosity | Moderate – allows glucose/insulin diffusion | High – engineered channels boost perfusion |
| Immune shielding | Effective for short‑term | Potentially long‑term with immunomodulatory cues |
| Scalability | Easy, low‑cost | Complex, requires bioprinter |
| Vascular integration | Limited | Designed for rapid angiogenesis |
Personalized medicine: Using patient‑specific iPSCs
Imagine taking a skin biopsy from a person with type 1 diabetes, re‑programming those cells into induced pluripotent stem cells (iPSCs), and then guiding them to become functional islets that perfectly match the patient’s immune profile. This autologous approach could dramatically lower rejection rates, though it raises cost and time considerations.
Key research gaps & upcoming trials
The field is buzzing with questions:
- How can we expedite beta‑cell maturation without sacrificing safety?
- What are the long‑term effects of a vascularized graft in a human body?
- Can we combine gene‑editing with bio‑ink to create “universal donor” islets?
Several phase‑I/II clinical trials are slated for 2025‑2027, focusing on safety, dosing, and graft durability. Keep an eye on trial registries if you’re interested in volunteering or following the results.
Staying Informed & Getting Involved
Follow breakthrough publications
Journals like Nature, Endocrine Reviews, and CellR4* regularly publish updates on islet biology. Subscribing to their alerts can give you a front‑row seat to the latest discoveries.
Join patient‑research consortia
Many nonprofit groups partner with labs to recruit trial participants, share data, and fund pilot studies. Being part of a community not only accelerates science but also provides emotional support from people walking the same path.
Support bioprinting research
Donations, advocacy, or simply spreading the word can help bring 3D‑printed islet technology out of the lab and into hospitals. Every bit helps turn a futuristic concept into a therapy that could change lives.
So, what do you think? Are functional human islets something you’d be excited to see in the clinic? If you have questions or want to dive deeper into any of the topics above, feel free to reach out. Together, we can keep the conversation alive and move closer to a world where diabetes is managed by a tiny, living organ rather than a handful of daily injections.
























Leave a Reply
You must be logged in to post a comment.