Hey there, friend. If you’ve just learned that you (or someone you love) have type 1 diabetes, the flood of questions can feel overwhelming—Will I ever feel normal again?What treatments actually work? Below, I’m breaking down the most current type 1 diabetes treatment landscape in a way that feels like a coffee‑chat, not a lecture. Grab a mug, settle in, and let’s explore how modern medicine, technology, and a few emerging therapies can help you stay healthy, active, and maybe even lighten the insulin load.
Core Treatment Pillars
Insulin – the Bedrock
Insulin is still the cornerstone of type 1 diabetes care. It replaces the hormone your pancreas can’t produce, keeping blood sugar in a safe range. In 2025 you’ve got more ways than ever to deliver it:
- Pens and vials – familiar, portable, and cheap.
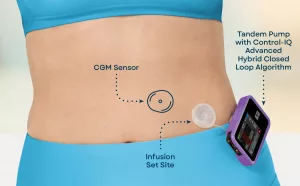
- Automated insulin delivery systems – these blend a CGM (continuous glucose monitor) with a smart pump that automatically adjusts basal rates. Want to learn the nuts‑and‑bolts? Check out our guide on automated insulin delivery.
- Hybrid closed‑loop pumps – often called “artificial pancreas” devices. They read glucose trends and give micro‑boluses without you lifting a finger.
Remember, more insulin isn’t always better. Too much can plunge you into hypoglycemia (those dreaded “low” episodes). Your endocrinologist will work with you to set a basal‑bolus ratio that matches your meals, activity, and daily rhythm.
Continuous Glucose Monitoring (CGM) & Hybrid Closed‑Loop
Imagine a tiny sensor under your skin that whispers your glucose numbers every five minutes. That’s a CGM. It lets you see patterns, not just single snapshots, so you can avoid big swings. When paired with a hybrid closed‑loop system, the algorithm takes the guesswork out of dosing.
According to a recent study from Breakthrough T1D, CGM users experience a 0.5 % drop in HbA1c and 40 % fewer severe hypoglycemia events. That’s the kind of real‑world benefit that turns numbers into freedom.
Immune‑Modulating Therapy – TZIELD
For the first time since insulin was discovered, a drug that actually targets the autoimmune attack behind type 1 diabetes is on the market. TZIELD (teplizumab) is a monoclonal antibody that slows the destruction of beta cells.
How does it work? It gently “re‑educates” the immune system so it stops firing at the insulin‑producing cells. The FDA granted it approval in 2023 after a pivotal trial showed a median delay of 2‑4 years before participants needed insulin. The drug’s own website explains that it’s given as a 14‑day IV infusion series.
Eligibility matters: you need to be in stage 2 (positive auto‑antibodies, abnormal glucose but not yet symptomatic) and at least 8 years old. It’s not a cure, but if you’re still making some C‑peptide, TZIELD can buy you precious time.
Off‑Label GLP‑1 Receptor Agonists – Semaglutide
When you hear “GLP‑1,” you probably think of type 2 diabetes. Yet many clinicians are now using semaglutide off‑label for type 1 patients who struggle with post‑meal spikes or need a gentle nudge on weight.
Here’s the quick rundown:
- Semaglutide & blood sugar: It modestly lowers HbA1c (0.3‑0.5 %) and smooths post‑prandial peaks. Read more about its impact on semaglutide blood sugar.
- Semaglutide & weight loss: For overweight or obese type 1 patients, the drug can shave off 5‑10 % of body weight, easing insulin resistance. Dive deeper at semaglutide weight loss.
- Semaglutide & type 1 diabetes: It’s not a replacement for insulin, but a supplement that may reduce total daily dose. Learn the nuances at semaglutide type 1 diabetes.
Safety first: GLP‑1s can raise the risk of ketoacidosis if insulin doses are cut too aggressively, so regular ketone checks are a must.
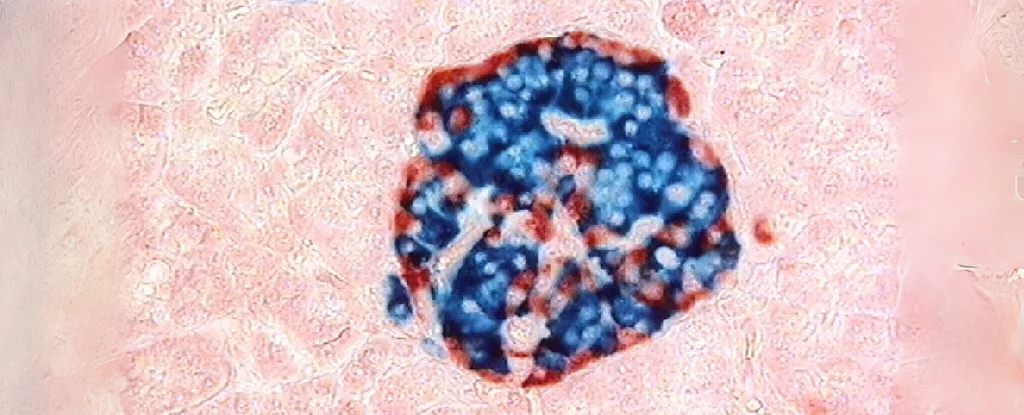
Emerging Cell‑Based & Regenerative Therapies
Stem‑cell and islet‑cell transplants have been in the news a lot lately. A 2024 clinical trial from the UK reported that two participants became insulin‑free after an islet‑cell transplant, while a third cut their insulin by 60 % within days. The key was a new monoclonal antibody (tegoprubart) that replaces traditional, toxic anti‑rejection drugs. Although still experimental, the results hint at a future where “pump‑only” could become reality.
Another FDA‑approved cellular therapy, Lantidra, is designed for patients who experience frequent severe hypoglycemia. While not yet mainstream, it shows the momentum toward curative approaches.
Choosing Your Mix
Assess Lifestyle & Goals
Do you thrive on structure or prefer a hands‑off vibe? If you love data, a CGM + hybrid closed‑loop might feel like a perfect match. If you’re often on the move and hate fiddling with devices, a reliable pen plus occasional pump “backup” could be simpler.
Medical Criteria to Consider
Age, disease stage, residual C‑peptide, and other health conditions shape your options. For example, if you still have measurable C‑peptide, you’re a good candidate for TZIELD. If you’re older and have cardiovascular concerns, discuss GLP‑1 use with your doctor.
Cost & Access
Insurance coverage varies widely. Insulin pumps and CGMs often qualify for reimbursement, while TZIELD may need prior authorization. Many manufacturers run patient‑assistance programs that can offset out‑of‑pocket costs. Don’t hesitate to ask your diabetes educator about “financial navigation” services.
Real‑World Snapshots
Case A – Teen on Hybrid Loop + Semaglutide: Sixteen‑year‑old Maya struggled with post‑lunch spikes. After adding a hybrid closed‑loop pump and low‑dose semaglutide, her HbA1c dropped from 7.8 % to 6.9 % and she lost 8 kg, giving her confidence to join the school soccer team.
Case B – Adult in Islet‑Cell Trial: David, 42, enrolled in a diabetes clinical trial for islet transplantation. Six months post‑procedure, he was insulin‑independent, and his CGM showed >70 % time‑in‑range—a life‑changing shift.
Balance Benefits & Risks
| Therapy | Key Benefit | Main Risk |
|---|---|---|
| Insulin (pens/pumps) | Immediate glucose control | Hypoglycemia if overdosed |
| CGM + Hybrid Loop | Reduced variability, less hypos | Device failure, skin irritation |
| TZIELD | Delays insulin need 2‑4 yr | Infusion reactions, infections |
| Semaglutide (off‑label) | Lower HbA1c & weight | Ketoacidosis if insulin cut too far |
| Islet‑Cell Transplant | Potential insulin independence | Immunosuppression side‑effects |
Common Pitfalls & How to Dodge Them
Hypoglycemia: If you’re tightening insulin, keep fast‑acting carbs on hand and set CGM alerts low at 70 mg/dL.
Ketoacidosis with GLP‑1: Never drop insulin below 0.1 U/kg without checking ketones. A simple urine strip can save a lot of trouble.
Infusion Reactions (TZIELD): Pre‑medication with antihistamines can reduce rash or fever. Report any fever >38 °C to your clinic immediately.
When to Switch
If your HbA1c stays above target despite diligent dosing, or if you experience frequent lows, it may be time to revisit your regimen. Likewise, if you feel “burned out” by constant finger sticks, consider moving to a hybrid system or discussing TZIELD eligibility.
Practical Toolkit Guide
Start‑A‑New‑Treatment Checklist
- Confirm disease stage with an auto‑antibody panel.
- Schedule a detailed consult with an endocrinologist—bring a list of questions (e.g., “Will I qualify for TZIELD?”).
- Check insurance coverage for pumps, CGM, and any novel therapies.
- Enroll in a training program: most hospitals offer pump‑school and CGM onboarding.
- Set up a daily log (paper or app) to track glucose, insulin, meals, and moods.
Helpful Resources & Community Support- National Diabetes Education Programs – free webinars on CGM use.
- Patient forums such as Diabetes.co.uk and JDRF community boards.
- Local diabetes camps – great for kids and teens to learn self‑management in a fun setting.
FAQ‑Style Quick Answers
What is the newest FDA‑approved therapy for T1D? TZIELD (teplizumab), approved in 2023, delays the need for insulin.
Can semaglutide replace insulin? No. It’s an adjunct that can improve glucose trends and aid weight loss, but insulin remains essential.
How does automated insulin delivery differ from a standard pump? A pump delivers preset rates; automated systems adjust those rates in real time based on CGM data.
Wrapping It All Up
Living with type 1 diabetes today feels nothing like the “take‑your‑insulin‑once‑a‑day” nightmare of the past. With reliable insulin, smarter devices, immune‑modulating drugs like TZIELD, and even off‑label GLP‑1 agents such as semaglutide, you can sculpt a treatment plan that fits your life, goals, and health status. The key is balance—understanding both the bright possibilities and the real risks. Talk openly with your care team, use the checklist above to stay organized, and don’t forget to lean on community resources for emotional support.
What do you think about the mix of technology and medication we’ve explored? Have you tried an automated insulin delivery system or considered a clinical trial? If any of these options sparked curiosity, let’s keep the conversation going. Your journey is unique, and you deserve a treatment plan that respects both your science and your story.




















Leave a Reply
You must be logged in to post a comment.