Short answer: yes. When your thyroid is over‑active it can press on the airway, swell, or even trigger a medication reaction that makes your throat feel raw. Ignoring it might mean missing a serious sign, so let’s unpack what’s really going on and what you can do about it.
Thyroid and Throat
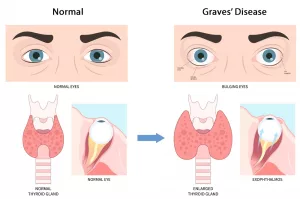
Goiter‑Induced Pressure
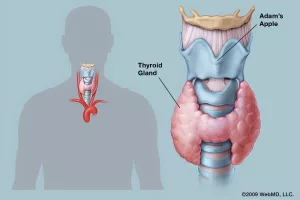
A goiter is simply an enlarged thyroid. Imagine a balloon inflating right behind your Adam’s apple – it can push against the trachea (the windpipe) and the esophagus (the food pipe). That pressure often feels like a lump in the throat, a tight band, or outright soreness when you try to swallow.
Typical signs include:
- A persistent “globus” sensation (like something is stuck in your throat)
- Occasional pain when swallowing food or liquids
- Feeling of tightness that worsens when you lie down
Most people notice these symptoms alongside classic hyperthyroidism symptoms such as rapid heartbeat, heat intolerance, weight loss, or tremors.
Thyroiditis‑Related Inflammation
Thyroiditis is inflammation of the thyroid gland. The most common form, viral or sub‑acute thyroiditis, often follows an upper‑respiratory infection. Within 24‑48 hours the thyroid can become tender, swollen, and painful. Because the gland sits so close to the throat, the pain radiates there.
What to look for:
- Sharp throat pain that peaks in a day or two and then eases
- Fever, fatigue, and aches that accompany the throat discomfort
- Temporary hyperthyroid signs (fast heart, anxiety) that later flip to hypothyroid signs (cold intolerance, sluggishness)
Most bouts resolve in a week or two, but if the pain lingers you may need an anti‑inflammatory like ibuprofen or, in severe cases, a short course of steroids—always under a doctor’s watch.
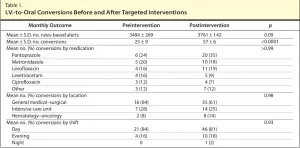
Medication‑Triggered Sore Throat
The drugs we use to tame an over‑active thyroid—mainly the thionamides carbimazole and propylthiouracil (PTU)—are usually well‑tolerated. However, a rare but scary side‑effect called agranulocytosis can appear suddenly. It’s a drop in white‑blood‑cell count that shows up as:
- High fever (often above 38 °C)
- Sore throat that won’t go away
- Persistent, sometimes hacking, cough
If you see any of these together, stop the medication immediately and call emergency services. The condition can progress quickly, but prompt treatment (often antibiotics and supportive care) leads to full recovery.
| Drug | Common Mild Side‑Effects | Rare Serious Side‑Effects |
|---|---|---|
| Carbimazole | Headache, rash, upset stomach | Agranulocytosis (fever, sore throat, cough) |
| Propylthiouracil (PTU) | Joint pain, nausea, dizziness | Agranulocytosis (fever, sore throat, cough) |
Other Causes
Infections
Most sore throats start as viral colds or bacterial strep. The clues that point to an infection rather than a thyroid issue are:
- Red, swollen tonsils with white patches
- Runny nose, sneezing, and overall “flu‑like” feeling
- Rapid improvement after a few days of rest or antibiotics (if bacterial)
If you have these signs, treat the infection first—but keep your thyroid medication schedule unchanged unless your doctor tells you otherwise.
Acid Reflux & LPR
Laryngopharyngeal reflux (LPR) is “silent” reflux that reaches the throat. It creates a burning sensation that mimics a sore throat, especially after meals or when lying down. Unlike a goiter, the discomfort often improves with antacids or lifestyle changes (e.g., no late‑night meals, raising the head of the bed).
Allergies & Post‑Nasal Drip
Seasonal allergies can cause clear mucus that drips down the back of the throat, leading to irritation and soreness. A quick antihistamine trial can help you decide if allergies are the culprit.
When to Seek
Red‑Flag Checklist
These signs should make you pick up the phone right now:
- Fever over 38 °C and sore throat
- Rapid heart rate (>100 bpm) combined with throat pain
- New hoarseness, difficulty breathing, or feeling like you can’t swallow
- Recent start or dosage change of a thionamide medication
What the Doctor Will Do
When you visit your clinician, expect:
- Physical exam: palpation of the neck to feel for goiter or tenderness
- Blood work: TSH, free T4, free T3, plus a full blood count to rule out agranulocytosis
- Ultrasound: if the gland feels enlarged or if you have persistent symptoms despite medication
Self‑Monitoring Tools
Keeping a simple log can save you trips to the ER. Record the date, temperature, throat pain level (1‑10), and any medication changes. Apps like “MyThyroidTracker” let you upload lab results and see trends over time.
Managing the Pain
Home Care (Low‑Risk)
These everyday tricks often give quick relief without messing with your thyroid meds:
- Warm salt‑water gargle 3‑4 times a day
- Honey‑lemon tea (no caffeine) to soothe the lining
- Stay hydrated—water, herbal teas, broths
- Humidify the air, especially in dry winter months
Targeted Treatments
Depending on the root cause, your doctor may suggest:
- Goiter‑related sore throat: Adjusting the anti‑thyroid dose, adding a beta‑blocker for symptom control, or exploring definitive treatments like radio‑iodine or surgery.
- Thyroiditis‑related pain: A short course of NSAIDs (ibuprofen) or, if pain is severe, a brief steroid taper.
- Medication‑induced: Immediate cessation of the thionamide, followed by a switch to an alternative (e.g., low‑dose radioactive iodine) after hematology clearance.
When Medication Adjustment Is Needed
If your sore throat persists despite the above, you may need a dose change. Talk openly with your endocrinologist about:
- Lowering the thionamide dose to reduce side‑effect risk
- Switching to another drug class if agranulocytosis is a concern
- Considering definitive therapy (radio‑iodine or thyroidectomy) if a large goiter continues to compress the airway
Real‑World Example
Emily, 34, came to the clinic with a three‑day sore throat, fever, and a new carbimazole prescription (30 mg daily). Her CBC showed a neutrophil count of 0.8 × 10⁹/L—classic agranulocytosis. She stopped the medication, was hospitalized, received antibiotics, and recovered in five days. Her endocrinologist later switched her to a lower‑dose PTU and monitored blood counts weekly. Emily’s story illustrates why rapid action can prevent a scary complication.
Expert Insights & Trusted Sources
For deeper reading, the American Thyroid Association offers evidence‑based guidelines on hyperthyroidism treatment. The NHS page details the range of thyroid medication side effects you should monitor.
Bottom Line Checklist
- Know whether your sore throat is from goiter, thyroiditis, or medication.
- Watch for fever + cough; if present, stop thionamides and seek emergency care.
- Keep a symptom diary and share it with your endocrinologist.
- Simple home remedies can ease discomfort while the underlying cause is treated.
Living with hyperthyroidism already feels like juggling a handful of symptoms—adding a sore throat can feel like an unexpected curveball. But with the right awareness, a few practical steps, and clear communication with your healthcare team, you can turn that uncomfortable feeling into a manageable signal. Got questions or a personal story to share? Drop a comment below or reach out to your doctor. Your throat (and your peace of mind) will thank you.






















Leave a Reply
You must be logged in to post a comment.