Most women notice more shedding or thinning as estrogen drops — and there are proven ways to stop it. Below you’ll find the fastest‑acting medications, gentle topicals, and low‑risk lifestyle tweaks, so you can choose the right menopause hair loss treatment for you.
Understanding Hair Loss
What causes hair loss during menopause?
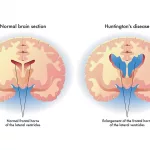
When you hit the perimenopause or post‑menopause stage, your body says goodbye to a lot of estrogen and progesterone. Those hormones normally keep hair follicles in the growth (anagen) phase, so when they dip, the follicles shrink, the growth cycle shortens, and hair ends up in the shedding (telogen) phase faster. At the same time, lower estrogen means the body produces relatively more male‑type hormones (androgens), and those androgens turn a friendly follicle into a shy one that stops growing as much. The whole process is often called “androgenic mini‑aturisation.”
How is it different from male‑pattern baldness?
Guys usually develop a distinct “M” shape with clear bald spots, while most women notice a more subtle, diffuse thinning across the crown and front. It’s slower, less dramatic, and often accompanied by a change in hair texture—not just a full‑on bald patch.
Which signs show it’s menopause‑related?
Typical clues include:
- Finding clumps of hair in your brush or shower drain.
- Gradual thinning on the top, sides, or front without any scaly patches.
- No itching, redness, or pain on the scalp.
- Feeling your hair feel finer or “silky‑ish” when you run your fingers through it.
If you notice any sudden patches, a scaly scalp, or pain, it might be something else—like alopecia areata or a skin condition—and a dermatologist should check it out.
What labs can confirm the cause?
A simple blood‑test panel can rule out other culprits and point you toward the right treatment. Most clinicians will order:
- Ferritin (iron stores) – iron deficiency is a sneaky cause of thinning.
- Thyroid panel (TSH, free T4) – hypothyroidism can mimic menopause‑related shedding.
- Sex‑hormone profile (estradiol, testosterone, DHEA‑S) – helps gauge the hormone imbalance.
- Vitamin D and B12 – low levels can affect hair health.
Having these numbers in hand makes it easier to pick a targeted menopause hair loss treatment rather than guessing.
Treatment Landscape
Topical Hair Treatments
Over‑the‑counter (OTC) options
Minoxidil 2 % (women’s strength) and 5 % (higher dose) are the only FDA‑approved topical treatments for female‑pattern hair loss. You apply it to a dry scalp twice a day, and after about 12–16 weeks you’ll often notice less shedding and a slight thickening. The trick is consistency—skip a day and the benefits disappear.
Prescription‑only topicals
Minomel Melatonin 0.1 % is a newer prescription solution that feeds follicles with an antioxidant. The melatonin helps protect the hair bulb from oxidative stress while the TrichoSol™ carrier delivers the active ingredient deep into the scalp. Users typically apply 1 ml once a day and see measurable regrowth in 4–6 months.
Botanical blends
Nutrafol’s Women’s Balance formula is a clinically‑studied, drug‑free blend that tackles six key drivers of menopausal thinning: hormonal imbalance, stress, inflammation, oxidative damage, nutritional gaps, and DHT sensitivity. The company cites several peer‑reviewed trials showing visible hair‑density improvements after 6 months of daily use (according to a 2024 clinical study). The formula includes saw palmetto (a natural DHT blocker), ashwagandha (stress‑relief), and the patented Synergen Complex that lowers cortisol, a hormone that can sabotage hair growth.
How to combine safely?
If you decide to run a minoxidil regimen alongside a prescription like melatonin, wait at least two hours between applications. This reduces the chance of scalp irritation and ensures each product can absorb properly.
Oral Hair‑Loss Medications
Finasteride & Dutasteride (off‑label)
These 5‑α‑reductase inhibitors trim down the conversion of testosterone to DHT, the most notorious androgen for hair follicle mini‑aturisation. Women usually need a low dose (0.5 mg for finasteride) and must use reliable contraception because the drugs can cause birth defects. Side effects may include decreased libido or mild breast tenderness.
Spironolactone
Spironolactone is a potassium‑sparing diuretic that also blocks androgen receptors. Doses range from 50–100 mg daily, and it can be a good bridge for women who can’t or don’t want to use finasteride. Watch the potassium level and have a baseline kidney function test.
Hormone Replacement Therapy (HRT)
Bioidentical estradiol (often combined with progesterone for women with a uterus) restores the estrogen environment that hair loves. Studies show that women on systemic HRT experience slower shedding and, in many cases, a modest increase in hair density (according to a 2023 review in the Journal of Menopause). HRT is not just a hair fix—it can also ease hot flashes, improve mood, and protect bone health. Talk to a menopause specialist to weigh benefits against risks like blood clots or breast‑cancer concerns.
Nutraceuticals & Supplements
Iron, zinc, biotin, omega‑3 fatty acids, and phyto‑estrogens (black cohosh, ginseng) all have varying degrees of evidence. Iron repletion is a must if ferritin is low—hair can bounce back quickly once iron stores normalize. Biotin is safe but only helpful when you actually lack it, which is rare.
When oral meds are off‑limits
If you have liver disease, a history of breast cancer, or are pregnant/breastfeeding, most oral anti‑androgens are contraindicated. In those cases, focus on topical options, supplements, and lifestyle changes.
Procedural & In‑Office Solutions
Platelet‑Rich Plasma (PRP)
PRP takes a small draw of your blood, spins it to concentrate platelets, and injects the plasma into the scalp. The growth factors stimulate dormant follicles and improve vascularisation. Most clinics recommend three sessions a month apart, followed by maintenance every 6–12 months. Costs can range from $500–$1,200 per session, so it’s a heftier investment but often yields noticeable thickening.
Low‑Level Laser Therapy (LLLT)
Hand‑held or cap‑style devices emit red‑light photons that boost cellular metabolism in hair follicles. The devices are FDA‑cleared for at‑home use; typical protocols call for 15‑30 minutes daily. The science is solid enough that many dermatologists suggest it as an adjunct to minoxidil.
Microneedling + topical absorption
A derma‑roller (0.5 mm needles) creates micro‑channels that let minoxidil or melatonin soak deeper. Studies show a 30 % higher hair‑count increase when microneedling is paired with topical medication.
Hair transplantation (FUE)
If thinning has progressed to a point where donor hair from the back of the scalp is still robust, follicular unit extraction (FUE) can move those follicles to areas of loss. It’s usually a last resort because the surgery is pricey and you still need to manage the underlying hormonal issue.
Lifestyle & Natural Adjuncts
Dietary patterns
Your hair is 90 % protein, so make sure you’re getting at least 1 g of protein per kilogram of body weight daily. Lean meats, legumes, Greek yoghurt, and tofu are great sources. Add antioxidant‑rich foods (berries, leafy greens) to combat oxidative stress, a hidden driver of hair loss.
Stress management
High cortisol levels can push hair follicles into telogen. Practices like gentle yoga, guided meditation, or even a 10‑minute evening walk can lower cortisol. Nutrafol actually measured cortisol drops in participants who followed a mindfulness routine alongside the supplement.
Scalp care habits
Switch to a sulfate‑free, pH‑balanced shampoo. Avoid tight ponytails, braids, or hair accessories that tug at the roots. When you brush, use a wide‑tooth comb and start at the ends, working your way up—this reduces breakage and stimulates gentle blood flow.
Alternative therapies
Acupuncture, TCM herbal formulas, and aromatherapy have anecdotal support for improving scalp circulation. A UK natural‑health blog notes that regular acupuncture sessions can lead to a modest reduction in shedding, though high‑quality clinical trials are still lacking.
Supplement checklist
| Supplement | Typical Dose | Key Benefit | Safety Note |
|---|---|---|---|
| Iron (if ferritin <30 µg/L) | 18 mg elemental iron daily | Replenishes iron stores, reduces telogen shift | Take with vitamin C; avoid if you have hemochromatosis |
| Zinc | 15–30 mg daily | Supports keratin synthesis | High doses can impair copper absorption |
| Biotin | 0.9 mg daily (RDA) | Helps keratin production | Excess rarely needed; may interfere with lab tests |
| Omega‑3 (fish oil or linseed) | 1–2 g EPA/DHA | Anti‑inflammatory, improves scalp health | Watch for blood‑thinning effect |
| Phyto‑estrogens (black cohosh, ginseng) | Based on product label | May modestly boost estrogen‑like activity | Discuss with doctor if on HRT |
Choosing the Right
Topical vs. oral – what fits you?
Consider these factors:
- Severity: Mild to moderate thinning often responds well to minoxidil or melatonin topicals. Severe, rapid shedding may need oral anti‑androgens or HRT.
- Skin sensitivity: If you have a flaky scalp, start with a gentle botanical blend before introducing minoxidil.
- Medical history: Liver disease, clotting disorders, or breast‑cancer risk tilt the balance toward topicals and lifestyle changes.
- Convenience: Topicals require twice‑daily application; oral meds are once‑daily but may need blood monitoring.
Balancing benefits and risks
Every treatment has a pro‑and‑con list. For example, finasteride can give impressive regrowth but may cause sexual side effects. Minoxidil is safe for most, but some people develop scalp irritation or unwanted facial hair. Making a decision chart can help you visualise which trade‑offs you’re comfortable with.
When to see a specialist?
If you notice any of the following, schedule a visit:
- More than 50 % of hair shedding in a month.
- Sudden patches, redness, or pain on the scalp.
- Accompanying symptoms like severe hot flashes, mood swings, or weight changes that suggest a broader hormonal shift.
- You want prescription‑only options (melatonin, oral anti‑androgens, or HRT).
Cost‑effectiveness comparison
| Option | Annual Cost (USD) | Typical Onset of Results | Insurance Coverage |
|---|---|---|---|
| Minoxidil 2 % (OTC) | $120 | 3–4 months | Usually not covered |
| Nutrafol Women’s Balance | $660 | 6 months | Rarely covered |
| Minomel Melatonin (prescription) | $240 (incl. doctor fee) | 4–6 months | Prescription‑only, private pay |
| Spironolactone (oral) | $150 | 2–3 months | Often covered |
| HRT (systemic) | $300–$800 | 2–3 months | Varies by plan |
| PRP (3 sessions) | $1,500–$2,400 | 4–6 months | Usually not covered |
Risks, Side Effects, & Safety
Common adverse events
Topicals can cause itching, dryness, or mild irritation—usually manageable with a gentle moisturizer. Oral anti‑androgens may lead to occasional nausea, breast tenderness, or a decrease in libido. HRT carries a well‑documented risk profile: increased clotting risk, a small rise in breast‑cancer incidence, and, for some, mood changes.
Serious warnings
Never combine oral finasteride with estrogen‑containing HRT without a doctor’s supervision—there’s a theoretical risk of excessive hormone fluctuation. If you’re on anticoagulants, be cautious with high‑dose omega‑3 supplements. And anyone with a personal or strong family history of hormone‑sensitive cancers should discuss alternatives like topical melatonin or PRP first.
Drug interactions
Spironolactone can increase potassium levels when taken with ACE inhibitors or potassium‑rich supplements. Minoxidil may heighten blood‑pressure‑lowering effects of antihypertensives, so keep an eye on your numbers if you’re on those meds.
Pregnancy & breastfeeding
All oral anti‑androgens (finasteride, dutasteride, spironolactone) are contraindicated during pregnancy because they can cause birth defects. Even topical minoxidil is generally avoided, especially in the first trimester. If you ever become pregnant, stop the medication and talk to your OB‑GYN right away.
Monitoring plan
Start with baseline labs, then re‑check every 3–6 months while on oral drugs. For topical users, schedule a follow‑up after 4 months to assess scalp tolerance and hair‑density changes. Keep a simple log: date, product used, any side effects, and notes on shedding. This personal data helps you and your clinician fine‑tune the regimen.
Bottom Line & Next Steps
Menopause‑related hair loss is not a sentence—it’s a signal that your hormones have shifted, and you have a toolbox of safe, evidence‑based treatments to bring the balance back. Begin with a quick blood‑test panel, then talk to a dermatologist or a menopause‑specialist about which combination of topical, oral, or procedural options feels right for your lifestyle and health profile. Remember, the most effective plan often blends a gentle topical (minoxidil or melatonin) with a targeted supplement (iron, zinc, or Nutrafol) and a few lifestyle tweaks that keep stress low and nutrition high.
If you’re ready to take the first step, click below to book a 15‑minute hair‑health consultation with our menopause‑focused clinician. Let’s turn the “shedding season” into a story of regrowth and confidence.
Schedule your free hair‑health review now























Leave a Reply
You must be logged in to post a comment.