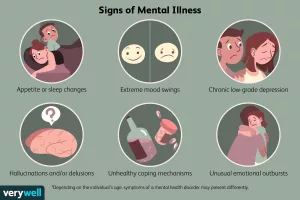
Hey there—if you’ve ever felt that a single weekly session isn’t enough, you’re not alone. So many of us juggle anxiety, low moods, or just that “something’s off” feeling, and the standard talk‑therapy model can feel a bit like trying to fix a leaky faucet with a single wrench. Below, I’m sharing the most practical mental health resources that go beyond the couch, from prescription medications to peer‑support circles. Think of this as a friendly guide you can dip into whenever you need a quick answer or a deeper dive.
Prescription Medications
Let’s start with the most common medical tool in the mental‑health toolbox: prescription medications. When a doctor prescribes an antidepressant, anti‑anxiety pill, or mood stabilizer, it’s usually after a careful assessment of your symptoms, medical history, and personal goals.
Types You’ll Hear About
- Antidepressants (SSRIs, SNRIs, tricyclics) – often the first line for depression and generalized anxiety.
- Anti‑anxiety medications (benzodiazepines, buspirone) – useful for short‑term relief of intense anxiety spikes.
- Mood stabilizers (lithium, valproate) – key for bipolar disorder and certain mood fluctuations.
Benefits and Risks
Medications can level the playing field, giving your brain a chance to reset so therapy and lifestyle changes work better. But they’re not magic pills. Common side effects range from mild nausea to more serious concerns like weight gain or sexual dysfunction. The risk of dependence is real for some drugs, especially benzodiazepines, so they’re typically prescribed for the shortest period possible.
Talking With Your Provider
Never shy away from asking questions. Here are a few you might keep handy:
- What exactly is this medication intended to do for me?
- How long before I might notice an effect?
- What side effects should I look out for?
- Are there interactions with other meds or supplements I’m taking?
According to the American Psychiatric Association, regular follow‑up appointments are essential to adjust dosage and monitor any adverse reactions.
Hospital Programs
When symptoms flare dramatically—think overwhelming panic, suicidal thoughts, or a psychotic break—hospital‑based care can be a lifesaver. But you don’t always need a full‑time stay; many facilities offer day programs or intensive outpatient services that let you keep living at home while receiving structured support.
Inpatient vs. Day Programs
- Inpatient admission provides 24/7 monitoring, medication management, and a safe environment during acute crises.
- Partial hospitalization (PHP) or intensive outpatient programs (IOP) involve several hours of therapy a day, several days a week, while you return home each night.
What Programs Offer
Typical services include cognitive‑behavioral therapy (CBT) groups, dialectical‑behavioral therapy (DBT) skills training, medication review, and sometimes creative art or movement therapy. The goal is to give you a structured routine and a team of professionals who can troubleshoot problems in real time.
Finding the Right Fit
Start by checking your insurance portal for “behavioral health” or “psychiatric” services. Many state health departments publish searchable directories of certified programs. The National Alliance on Mental Illness (NAMI) maintains a helpful locator that you can filter by location and type of care. When you call, ask about:
- Average length of stay or program duration
- Staff credentials (psychiatrists, licensed therapists, peer specialists)
- Family involvement policies
- After‑care follow‑up plans
Mind‑Body Interventions
If you’ve ever felt a wave of calm after a short breathing exercise, you already know the power of mind‑body work. These practices teach the nervous system to shift out of “fight‑or‑flight” mode and into a more relaxed, focused state.
Popular Practices
- Yoga – gentle movement synced with breath, proven to lower cortisol.
- Mindfulness meditation – observing thoughts without judgment, often using apps.
- Tai‑chi and Qigong – slow, flowing motions that combine stretch, balance, and breath.
- Progressive muscle relaxation – systematically tensing and releasing muscle groups.
Science Backing the Benefits
A meta‑analysis published in JAMA Psychiatry found that regular mindfulness practice reduced symptoms of anxiety and depression by an average of 30 % compared with control groups. Similarly, a Harvard Health study highlighted yoga’s ability to improve mood and sleep quality, especially when practiced at least three times per week.
Free Tools and Apps
Not ready to buy a pricey subscription? Try these no‑cost options:
- Breathe – a simple web‑based mindfulness timer.
- Pixel Thoughts – a 60‑second guided “brain dump” to clear racing thoughts.
- Headspace – offers a free introductory meditation series.
Peer Support Groups
There’s something profoundly healing about knowing you’re not the only one navigating a particular mental health maze. Peer support groups give you a safe space to share, learn, and feel understood without the pressure of formal therapy.
Why They Work
Human beings are wired for connection. Hearing a story that mirrors your own can validate feelings that seemed “odd” or “isolated.” Research from the National Institute of Mental Health shows that participants in peer‑led groups report higher treatment adherence and lower relapse rates.
Where to Find Them
- Online chat & text – Crisis Text Line lets you text HOME to 741741 for confidential, volunteer‑run support.
- LGBTQ+ youth – The Trevor Project offers 24/7 counseling and peer forums.
- General community – NAMI’s local support‑group directory connects you with in‑person or virtual meetings.
Choosing the Right Group
Ask yourself these quick questions before you jump in:
- Is the group moderated by a trained facilitator?
- Do members share similar experiences (e.g., depression, PTSD, substance use)?
- Is the environment confidential and respectful?
Crisis Resources
Even with the best long‑term plan, moments of acute distress happen. Knowing how to get help fast can make all the difference.
When to Reach Out
If you ever feel you might act on self‑harm thoughts, hear voices that tell you to hurt yourself, or you’re in a situation that feels unsafe, call emergency services (911 in the U.S.) or go to the nearest emergency department.
Hotlines You Can Trust
- 988 – the U.S. Suicide and Crisis Lifeline, 24/7, free.
- Text HOME to 741741 – connects you to a Crisis Text Line volunteer.
- National Suicide Prevention Lifeline – 1‑800‑273‑8255 (also offers live chat).
Quick Safety Checklist
- Identify a safe place (friend’s house, public space).
- Keep a list of crisis contacts on your phone.
- Remove or lock away any means you might use for self‑harm.
- Reach out immediately—don’t wait for the feeling to pass.
Build Your Personal Toolkit
Now that we’ve explored the big categories, it’s time to blend them into a personalized “toolkit.” Think of it as a menu you can pick from depending on the day, your mood, and your goals.
Self‑Assessment Questions
- What symptom feels most pressing right now? (e.g., insomnia, racing thoughts, low motivation.)
- Do I have a prescriber I trust, or do I need to start that conversation?
- Would a structured program (hospital or day‑program) help me create routine?
- Am I comfortable sharing in a peer group, or would I start with online text support?
- Which mind‑body practice sounds enjoyable, not like a chore?
Combining Resources – Sample Plan
| Resource | Goal | How to Use It |
|---|---|---|
| Prescription medication (SSRI) | Stabilize mood & reduce anxiety | Take daily as prescribed; schedule follow‑up in 4–6 weeks |
| Intensive outpatient program | Build coping skills & structure | Attend 3‑hour group sessions Mon‑Thu; practice skills at home |
| Mindful breathing (Breathe app) | Quick anxiety relief | 2‑minute breathing exercise when thoughts race |
| Peer support text line | Feel heard in the moment | Text “HOME” to 741741 during a crisis or low‑energy day |
| Yoga (YouTube beginner series) | Improve sleep & body awareness | 10‑minute stretch before bedtime, 3×/week |
Expert Tips for Success
Clinical psychologists often recommend “stacking” low‑effort habits first (like a 2‑minute breath) before tackling bigger commitments (like a weekly therapy slot). This stacking creates momentum and makes the whole system feel doable.
Putting It All Together
Remember, mental health isn’t a single‑choice menu; it’s a buffet. You can try a little of everything, see what sticks, and adjust as you grow. Here’s a quick recap of the pillars we covered:
- Prescription medications – consider them when biology needs a boost.
- Hospital and day programs – provide structure and intensive skill‑building.
- Mind‑body interventions – empower your nervous system with breath, movement, and mindfulness.
- Peer support groups – give you community, validation, and practical tips.
- Crisis resources – keep numbers handy for those “just in case” moments.
What matters most is that you feel heard, supported, and equipped to navigate the ups and downs. If you’re ready to take a tiny step today, why not text HOME to 741741 for a quick, confidential chat? Or open the Breathe app and try a single 2‑minute session right now.
We’re all on this journey together, and sharing what works (or what didn’t) helps everyone. Feel free to drop a comment below about the resources you’ve tried, ask questions, or just say hi. You deserve a mental‑health toolbox that feels as unique as you are.























Leave a Reply
You must be logged in to post a comment.