Congrats—you’ve crossed the menopause finish line, and now you’re stepping into the post‑menopausal chapter. What does this mean for your body, your mood, and your day‑to‑day life? In a nutshell, your hormones settle at a lower level, which can raise the odds of a few health bumps, but it also opens a window for new habits that keep you feeling strong, vibrant, and confident.
Below you’ll find the most practical, science‑backed advice for navigating heart health, bone health, mental well‑being, nutrition, exercise, and preventive screenings. Think of this as a friendly conversation over coffee—no jargon, just clear guidance and a few personal stories to keep things real.
What is postmenopausal health?
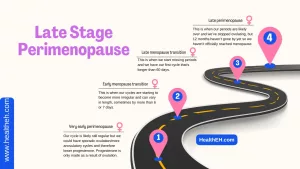
Definition and timeline
Postmenopause officially begins after you’ve gone 12 consecutive months without a period. It’s not a “disease” but a natural stage of women’s health. On average, women hit this milestone around age 51, but you might notice it a little earlier or later—both are perfectly normal.
Hormonal landscape
During this phase, estrogen and progesterone levels stay low. Without estrogen’s protective hug, blood vessels can stiffen a bit, and bone‑remodeling speeds up. That’s why we pay extra attention to cardiovascular and bone health after menopause.
Why it matters – risk vs. benefit
Low estrogen reduces the risk of hormone‑sensitive cancers, but it also nudges up the chances of heart disease, osteoporosis, and mood swings. The good news? Most of those risks can be managed with lifestyle tweaks and regular check‑ups.
Heart health matters most
How estrogen protects the heart
Estrogen helps keep arteries flexible, boosts “good” HDL cholesterol, and softens the buildup of “bad” LDL. When estrogen drops, those protective effects wane, and heart disease risk begins to climb—by your 70s, women’s heart disease rates catch up to men’s, according to the Office on Women’s Health.
What changes after menopause?
Blood pressure may rise a bit, cholesterol profiles shift, and the heart works a little harder. If you add other factors—smoking, sedentary lifestyle, family history—the risk can increase significantly.
Screening & risk‑stratification
Every 3‑5 years, use the ACC/AHA pooled‑cohort risk calculator (ACC/AHA estimator) to see where you stand. It’s a quick online tool that gives you a 10‑year risk percentage for heart attack or stroke.
Prevention strategies
- Nutrition: Adopt a Mediterranean‑style diet—lots of fruits, vegetables, whole grains, fish, nuts, and olive oil. Keep sodium under 2 g per day.
- Exercise: Aim for at least 150 minutes of moderate‑intensity cardio (brisk walking, cycling, swimming) plus two strength‑training sessions each week.
- Medical options: If you’re high‑risk, a low‑dose statin may be recommended, and some doctors suggest a daily low‑dose aspirin for selected women (USPSTF guidance).
Bone health and osteoporosis
Why bone loss accelerates
Estrogen tells bone‑building cells (osteoblasts) to keep working and tells bone‑breaking cells (osteoclasts) to slow down. Without it, the balance tips toward loss, and bone density can drop 1‑2 % per year.
Calcium & vitamin D recommendations
Aim for 1,200 mg of calcium and 800–1,000 IU of vitamin D daily. Dairy, fortified plant milks, leafy greens, and a sensible supplement can help you hit those numbers.
Screening: DEXA scan timing
Start bone density testing at age 65, or earlier if you have risk factors—family history of fractures, low body weight, smoking, or prolonged steroid use. A DEXA scan is painless and gives a clear picture of your bone health.
Pharmacologic options
If your DEXA shows low bone mass, doctors may prescribe bisphosphonates (like alendronate), denosumab, or, in certain cases, low‑dose hormone therapy. The choice depends on your overall risk profile and preferences.
Weight‑bearing exercise plan
Simple activities such as brisk walking, dancing, stair climbing, or resistance band workouts can curb bone loss. Aim for at least 30 minutes of weight‑bearing activity most days of the week.
Mental and hormonal balance
Mood swings, anxiety & depression
About 20 % of postmenopausal women report moderate to severe depressive symptoms. The hormonal dip, sleep disturbances, and life transitions all play a part. If you notice persistent low mood, a talk with your primary care provider or a mental‑health professional is a smart move.
Vaginal health & sexual function
Low estrogen can cause vaginal dryness and mild pain during intimacy. Over‑the‑counter lubricants work for many, while low‑dose vaginal estrogen creams (prescribed by a doctor) can restore comfort for others.
Hormone‑therapy (HT) – pros & cons
HT can melt away hot flashes, protect bone, and improve mood, but it isn’t for everyone. It’s safest for women who start it within 10 years of menopause and have a low baseline risk for blood clots or breast cancer. Discuss benefits and risks with a board‑certified OB‑GYN to decide if it’s right for you.
Non‑pharmacologic coping tools
Mindfulness meditation, cognitive‑behavioral therapy (CBT), regular sleep routines, and staying socially active have all been shown to lift mood and ease anxiety during the postmenopausal years.
Nutrition you’ll actually enjoy
Core food groups
Think color and variety: whole grains, legumes, leafy greens, berries, fatty fish (rich in omega‑3s), and nuts. These foods supply fiber, antioxidants, and heart‑friendly fats.
Managing weight gain
Metabolism naturally slows a bit after menopause. A modest daily calorie reduction of 200‑300 kcal, combined with higher protein intake (about 1 g/kg body weight), helps preserve muscle while keeping the scale honest.
Foods to limit
Cut back on processed meats, sugary drinks, and trans‑fats. Excess sodium can raise blood pressure, and added sugars can spike insulin, both of which stress the cardiovascular system.
Sample 7‑day meal plan
| Day | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Mon | Greek yogurt with berries & chia | Quinoa salad with chickpeas, spinach, feta | Grilled salmon, roasted broccoli, sweet potato |
| Tue | Oatmeal topped with walnuts & banana | Turkey wrap with avocado, mixed greens | Stir‑fried tofu, brown rice, mixed veggies |
| Wed | Scrambled eggs, whole‑grain toast, sliced tomato | Lentil soup, side kale salad | Chicken breast, quinoa pilaf, sautéed asparagus |
| Thu | Smoothie (spinach, almond milk, frozen mango, protein powder) | Greek salad with grilled shrimp | Beef stew with carrots & potatoes (lean cut) |
| Fri | Whole‑grain English muffin, peanut butter, apple slices | Veggie‑packed chili | Baked cod, couscous, steamed green beans |
| Sat | Protein pancakes, fresh berries | Caprese sandwich on whole‑grain bread | Veggie lasagna with ricotta, side mixed salad |
| Sun | Fruit parfait with granola | Grilled chicken Caesar (light dressing) | Roasted turkey, quinoa‑wild rice blend, roasted carrots |
Exercise prescription for postmenopausal women
Aerobic vs. resistance vs. flexibility
A balanced routine includes:
- Aerobic: 150 minutes of moderate activity (walking, swimming, cycling) weekly.
- Resistance: Two to three sessions of weight training or body‑weight exercises to preserve muscle mass and bone density.
- Flexibility: Yoga or gentle stretching 2‑3 times a week to keep joints supple and reduce stress.
Dos and don’ts (from a NCBI study)
Do focus on weight‑bearing activities that challenge your bones, like brisk walking, dancing, or light jogging. Don’t dive into high‑impact workouts if you have severe osteopenia without a professional’s green light.
Safety checklist
- Get a medical clearance if you’ve been sedentary for a while.
- Invest in supportive shoes—your joints will thank you.
- Start slowly, then gradually increase intensity and load.
- Listen to your body; soreness is okay, sharp pain is not.
Preventive screenings & vaccinations
| Screening | When to start | Frequency | Key source |
|---|---|---|---|
| Mammogram | Age 40 (or 10 years before earliest family case) | Every 1‑2 years | USPSTF |
| Pap/HPV | Age 21 | Every 3 years (HPV‑primary) | CDC |
| Colorectal | Age 45 | Every 10 years (colonoscopy) | USPSTF |
| Bone density (DEXA) | Age 65 (earlier with risk) | Every 2‑5 years | AAFP |
| Blood pressure | Age 18 | Every 1‑2 years | HHS |
| Lipid panel | Age 45 (earlier with risk) | Every 4‑6 years | ACC/AHA |
| Flu vaccine | Every season | Annually | CDC |
| COVID‑19 booster | As recommended | According to CDC schedule | CDC |
Real‑world experiences: stories that stick
Case study #1 – Heart health turnaround
Emily, 58, was diagnosed with borderline high cholesterol during her routine check‑up. She swapped sugary snacks for a Mediterranean eating plan, added a 30‑minute evening walk, and started a low‑dose statin. Six months later, her LDL dropped 30 % and she feels more energetic than she did in her early 50s.
Case study #2 – Bone density rescue
Laura, 62, discovered mild osteopenia on a DEXA scan. Her doctor prescribed calcium, vitamin D, and a weekly bisphosphonate. She also began two strength‑training sessions per week. After two years, her bone density stabilized, and she avoided any fractures despite leading an active lifestyle.
Reader‑submitted tip
“I started a 15‑minute morning yoga routine after menopause, and it’s been a game‑changer for my mood and flexibility,” writes Maya, 55. Small, consistent habits can add up to big health dividends.
Wrapping it all up
Postmenopausal health isn’t about fearing the future; it’s about empowering yourself with knowledge, supportive habits, and regular check‑ins. Focus on three pillars: keep your heart humming, protect your bones, and nurture your mental well‑being. Pair those pillars with a balanced diet, enjoyable movement, and the recommended screenings, and you’ll set the stage for many vibrant, healthy years ahead.
Ready to take the next step? Download our free “Postmenopausal Health Checklist” (linked at the end of the article) and start ticking off the actions that feel right for you. Got questions, anecdotes, or a favorite recipe to share? Drop a comment below—let’s keep the conversation going!























Leave a Reply
You must be logged in to post a comment.