Hey there! If you’ve ever wondered why your big toe suddenly feels like it’s on fire or why your knee swells out of nowhere, you’re not alone. Gout and calcium‑pyrophosphate deposition disease (CPPD) are the two biggest culprits behind those sharp, unexpected joint pains. They’re both crystal‑driven, but the crystals are different, and that means the tricks we use to calm the inflammation differ, too. In the next few minutes we’ll walk through what these diseases look like, why they happen, and what you can actually do about them—no jargon, just friendly advice.
Overview
What Are Gout and CPPD?
Gout happens when monosodium urate (MSU) crystals pile up in the joint space. Think of it as tiny, sharp needles that the body’s immune system can’t ignore. CPPD, often called “pseudogout,” is caused by calcium‑pyrophosphate dihydrate (CPP) crystals that settle in cartilage and joint fluid. Both are types of crystal‑driven inflammation, but the chemical makeup of the crystals determines which pathways light up in our immune cells.
Why Group Them Together?
Because they share a lot of ground: sudden swelling, intense pain, and a common hero in the story – the macrophage. In gout, macrophages unleash the NLRP3 inflammasome, releasing IL‑1β and a cascade of painful signals. In CPPD, they fire a slightly different set of alarms that still end in inflammation, just via a separate lysosomal route (the exact details are still being untangled by researchers). This overlap is why doctors often test for both at the same time.
Key Numbers
Gout affects roughly 3‑8 % of adults in the United States, with men over 65 being the most common. CPPD is sneaky – up to half of people over 85 have CPP crystals in their knees, even if they never feel a flare. The bottom line? Both are far more common than you might think.
Pathophysiology
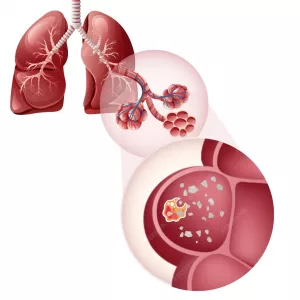
Macrophage Pathways in Gout
When MSU crystals land in the joint, they are recognized as danger signals. Macrophages swallow them, their lysosomes burst, and the NLRP3 inflammasome lights up. The result? A surge of interleukin‑1β that recruits neutrophils, causing the classic hot, red, painful joint.
Macrophage Pathways in CPPD
CPP crystals also get gulped by macrophages, but the response leans more on lysosomal destabilization without the same NLRP3 dominance. Instead, other cytokines (like IL‑6) take center stage, leading to an inflammation pattern that can mimic rheumatoid arthritis or osteoarthritis.
Environmental Triggers
There’s growing evidence that exposure to certain toxic particles—think silica dust from construction sites—primes macrophages, making them more likely to over‑react when crystals appear. For a deeper dive on that link, check out the article on toxic particle diseases. It’s a reminder that what we breathe can influence what hurts our joints.
Risk Factors
Shared Risks
Age, genetics, and an overall metabolic “sweet spot” are the biggest shared risk factors. As we get older, cartilage changes, and the balance of minerals in the joint fluid shifts, paving the way for crystal formation.
Gout‑Specific Triggers
High serum uric acid (hyperuricemia) tops the list. Diets rich in purines—red meat, shellfish, and especially alcohol—push uric acid levels up. Dehydration, obesity, and certain medications (like diuretics) also tip the scale.
CPPD‑Specific Triggers
Joint trauma (including knee surgery), metabolic disorders such as hemochromatosis or hyperparathyroidism, and low magnesium levels can nudge CPP crystals into existence. Even chronic exposure to silica (the same culprit behind silicosis) can play a role—read more about silicosis causes if you’re curious.
Real‑World Snapshot
Imagine a 68‑year‑old former construction worker who’s been dealing with knee stiffness for years. He finally gets a sudden, sharp knee pain after a garden spade accident. After a joint‑fluid tap reveals CPP crystals, his doctor explains that the long‑term silica exposure may have set the stage for his flare. That story isn’t rare; it’s a perfect illustration of how environment and biology intersect.
Clinical Presentation
Typical Gout Attack
The classic “podagra” (big‑toe gout) starts with a sudden, blistering pain that peaks within a few hours. The joint becomes red, hot, and swollen. While the toe is the most common launch site, you can also see gout in the ankle, knee, wrist, or fingers.
Typical CPPD Flare
CPPD loves the knee, wrist, and ankle. The pain can feel like a deep, throbbing ache that may involve more than one joint at a time. Some patients even develop a “crowned‑dens” pain in the neck when CPP crystals settle in the cervical spine ligaments.
Overlap Symptoms
Both conditions share warmth, swelling, limited motion, and sometimes low‑grade fever. That’s why a simple “look‑and‑feel” exam isn’t enough—you need that crystal check.
| Feature | Gout | CPPD (Pseudogout) |
|---|---|---|
| Typical joint | Big toe (podagra), ankle, knee | Knee, wrist, ankle, cervical spine |
| Crystal type | Monosodium urate (needle‑shaped) | Calcium‑pyrophosphate dihydrate (rhomboid) |
| Onset | Within minutes, peaks in hours | Hours to days, may involve multiple joints |
| Associated conditions | Hyperuricemia, obesity, alcohol | Joint trauma, hemochromatosis, hyperparathyroidism |
| Typical imaging | Double‑contour sign on US | Chondrocalcinosis on X‑ray |
Diagnosis
Joint‑Fluid Analysis
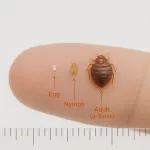
The gold standard for both diseases is a tap of the affected joint. Under polarized light microscopy, gout shows needle‑shaped, negatively birefringent crystals, while CPPD displays rhomboid, positively birefringent crystals. This test settles the “is it gout or pseudogout?” question quickly.
Imaging
Standard X‑rays can reveal chondrocalcinosis—a tell‑tale calcification of cartilage in CPPD. Ultrasound is great for spotting the “double‑contour” sign of MSU crystals in gout. MRI isn’t usually needed unless you suspect spinal involvement.
Blood Work
Checking serum urate levels helps confirm gout but isn’t definitive (levels can be normal during an attack). For CPPD, you’ll often screen for calcium, magnesium, iron, and parathyroid hormone to catch underlying metabolic drivers.
When to Look Deeper
If you have recurrent flares without an obvious cause, ask your doctor to rule out secondary issues—like hyperparathyroidism or hemochromatosis. Those conditions can be silently fueling the crystal storm.
Treatment
Acute Flare Management
Whether you’re battling gout or CPPD, the first‑line weapons are the same: NSAIDs (like ibuprofen), colchicine, or corticosteroids (oral or injected straight into the joint). The key is to start treatment early—ideally within the first 12 hours—to blunt the inflammatory cascade.
Gout‑Specific Long‑Term Care
Urate‑lowering therapy (ULT) is the cornerstone. Allopurinol and febuxostat reduce serum uric acid, preventing new crystal formation. Lifestyle changes—cutting back on red meat, alcohol, and sugary drinks—also make a big difference.
CPPD‑Specific Long‑Term Care
Unfortunately, we don’t have a drug that dissolves CPP crystals. Management focuses on controlling inflammation (same NSAIDs, colchicine, steroids) and treating any underlying metabolic disorder. Some clinicians use low‑dose colchicine prophylactically if flares are frequent.
Emerging Therapies
Targeting the IL‑1 pathway (think anakinra or canakinumab) has shown promise for refractory gout and is being explored for CPPD. A 2023 clinical trial (cited a study) reported faster pain resolution with IL‑1 blockade in gout patients who couldn’t tolerate NSAIDs.
Lifestyle Tweaks
For gout, staying hydrated, maintaining a healthy weight, and limiting purine‑rich foods can lower uric acid. For CPPD, ensuring adequate magnesium intake (leafy greens, nuts) and avoiding excessive calcium supplements can help. Simple moves like gentle low‑impact exercise keep joints limber without triggering flares.
Overlap & Differential Diagnosis
Mixed Crystal Disease
Yes, it’s possible to have both MSU and CPP crystals at once—a condition called mixed crystal arthritis. It’s rare but worth remembering if you have atypical flares that don’t respond to standard therapy.
Distinguishing From Other Arthritides
Septic arthritis, rheumatoid arthritis, and osteoarthritis all can look similar. Key red flags for infection include fever >38 °C, rapid joint destruction on imaging, and a purulent joint fluid. Rheumatoid arthritis usually shows symmetric polyarthritis and positive rheumatoid factor, while osteoarthritis presents with chronic, wear‑and‑tear changes without the intense acute inflammation.
Lifestyle & Prevention
Nutrition for Gout
Cut back on organ meats, anchovies, and sugary beverages. Cherry juice and vitamin C have modest urate‑lowering effects. Pair that with a daily water intake of at least 2‑3 L, and you’ll give your kidneys a better chance to flush uric acid.
Nutrition for CPPD
Focus on magnesium‑rich foods (pumpkin seeds, whole grains) and keep calcium intake balanced—not too low, not too high. If you have hyperparathyroidism, your endocrinologist will guide you on safe calcium levels.
Exercise & Joint Care
Low‑impact activities—walking, swimming, cycling—keep joints moving without over‑loading them. Strengthening the quadriceps can help support the knee, a common site for CPPD flares.
Environmental Awareness
If you work in construction, mining, or any field with dust exposure, use proper respiratory protection. Those macrophage pathways can be sensitized by inhaled particles, making crystals more likely to cause trouble later on.
Conclusion
Gout and CPPD may feel like unwelcome guests that show up without warning, but understanding what drives them—crystals, macrophages, and the body’s own chemistry—gives you the power to manage and even prevent future attacks. Whether you’re reaching for the ibuprofen bottle, sipping cherry juice, or planning a doctor’s visit for a joint‑fluid tap, each step you take brings you closer to a life where joint pain isn’t the star of the show.
Got questions about your own flares? Wondering how to tweak your diet or which medication might be right for you? Feel free to explore the internal resources linked throughout this article, and remember: you don’t have to navigate crystal‑driven inflammation on your own. Let’s keep the conversation going—after all, sharing experiences is the best way to turn knowledge into real‑world relief.






















Leave a Reply
You must be logged in to post a comment.