Imagine trying to say a simple sentence, but your tongue and lips feel like they’ve misplaced their choreography. You know what you want to say, yet the sounds stumble out, slow and tangled. That’s exactly what people with progressive apraxia of speech (PAOS) experience – a neuro‑degenerative disruption of the brain’s speech‑planning system. In the next few minutes we’ll walk through what PAOS is, how it unfolds, why it matters, and what you can actually do about it. Grab a cup of tea, settle in, and let’s explore this together.
What Is PAOS?
PAOS is a rare disorder where the brain’s “motor‑programming” network fails to translate thoughts into smooth speech movements. Unlike a stroke that suddenly knocks out speech, PAOS creeps in quietly, often as the sole symptom for years. The hallmark signs are:
- Groping or “searching” movements of the lips and tongue.
- Slow, effortful speech, especially on multisyllabic words.
- Frequent sound substitutions (“gasket” becomes “dasket”).
The condition usually begins in adulthood, with prevalence under one per million (Orphanet). Because it can be the only observable deficit for a long time, many doctors initially miss it or label it simply as “dysarthria.”
PAOS vs Other Disorders
To keep the picture clear, let’s compare PAOS with a few look‑alikes.
| Feature | PAOS | Dysarthria | Non‑fluent PPA | Stuttering |
|---|---|---|---|---|
| Root problem | Motor‑planning deficit | Motor‑execution deficit | Language‑plus speech deficit | Fluency control |
| Typical onset | Adult, gradual | Any age, sudden or progressive | Adult, progressive | Childhood |
| Key symptom | Groping, sound errors | Weak, imprecise articulation | Agrammatism + AOS | Repeats, blocks |
Another common confusion is with Parkinson‑like syndrome. Both can present with stiff, slow movements, but PAOS primarily hits speech planning, while Parkinsonian features involve broader motor control.
How It Progresses
Early on, you might notice only a slight hesitation on longer words. Over months to years, the effort intensifies, and additional signs may appear:
- Year 0‑2: Isolated speech‑planning difficulty.
- Year 2‑5: Subtle word‑finding pauses, occasional dysphagia (swallowing trouble).
- Year 5‑8: Emerging mild aphasia or memory lapses, possible motor signs resembling Parkinsonism.
Research by Josephs et al. (2014) showed that “AOS can be the only observable deficit for a number of years,” underscoring the need for vigilance. Eventually, underlying pathology—often tau pathology or TDP‑43 proteinopathy—drives broader cognitive and motor decline.
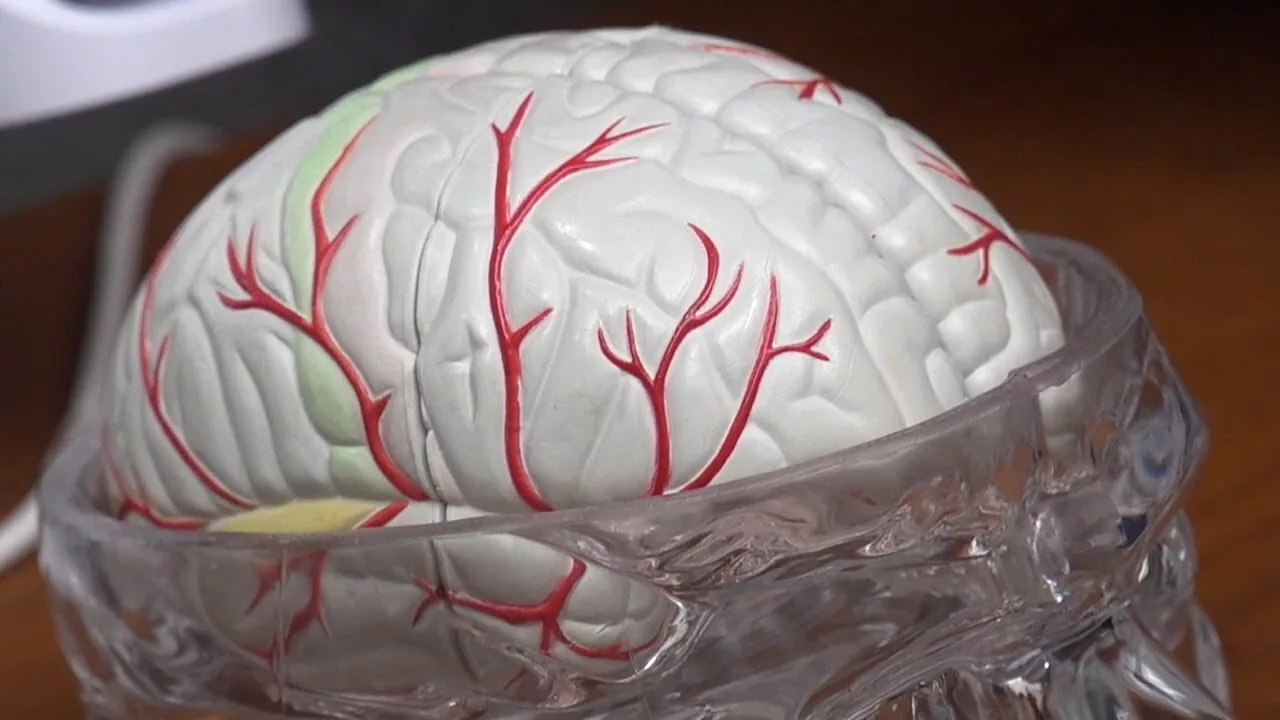
Brain Changes & Pathology
The brain regions first hit are the left posterior frontal cortex and supplementary motor area—areas that orchestrate the precise timing of speech muscles. Imaging studies consistently reveal atrophy or reduced metabolism in these zones.
Two major protein culprits have been identified:
- Tau pathology: Frequently linked to progressive supranuclear palsy or corticobasal syndrome. Tau aggregates can be visualized with specialized PET tracers.
- TDP‑43 pathology: Often associated with frontotemporal lobar degeneration.
Recent advances in neuroinflammation PET imaging allow researchers to see microglial activation even before structural changes appear. This opens doors for early detection and potential anti‑inflammatory interventions.
Diagnosis & Assessment
Getting a solid diagnosis usually involves three steps:
- Clinical speech evaluation: Speech‑language pathologists use tasks like rapid repetition of multisyllabic strings, assessing for groping and sound errors.
- Neuroimaging: MRI to rule out stroke or tumor; FDG‑PET to spot frontal hypometabolism; optionally tau‑PET or neuroinflammation PET for research settings.
- Biomarkers (emerging): CSF tau, neurofilament light chain, and even blood‑based markers are being validated.
If you or a loved one shows the early signs, ask your neurologist for a referral to a specialized speech‑language clinic. Early detection not only aids planning but also opens the door to therapy that can preserve communication for longer.
Management & Care
While there’s no cure yet, a proactive, multidisciplinary approach can make a real difference.
Speech‑Language Therapy
Intensive motor‑programming programs, like the “MAX” protocol, have demonstrated modest slowing of speech decline (Utianski et al., 2018). The key is high‑frequency practice—think of it as a daily “speech workout.” Here are a few home tips:
- Chunk longer words into syllables and practice slowly, then gradually speed up.
- Record yourself and listen for improvements; it’s a great confidence booster.
- Use visual cues (mirror or app) to monitor mouth shape.
Pharmacologic Options
At present, medication targets secondary symptoms. If Parkinson‑like rigidity appears, low‑dose levodopa may help. Ongoing trials are testing anti‑tau antibodies—keep an eye on clinical trial registries for enrollment opportunities.
Swallowing & Nutrition
As PAOS progresses, dysphagia can develop. A bedside swallowing assessment by a speech therapist is essential. Recommendations often include soft‑texture foods, thickened liquids, and upright posture during meals.
Support for Caregivers
Living with PAOS reshapes daily life for the whole family. Encourage caregivers to join support groups, seek counseling, and practice self‑care. Small rituals—like a weekly “chat” over coffee—can maintain emotional connection.
Key Takeaways
Progressive apraxia of speech is a rare but impactful neurodegenerative condition that strikes the brain’s speech‑planning circuitry. It often starts as the lone symptom, making early recognition crucial. Typical brain changes involve the left frontal motor network and may be driven by tau pathology or TDP‑43 proteinopathy, sometimes accompanied by brain inflammation. A combination of detailed speech assessment, advanced imaging—including neuroinflammation PET imaging—and emerging biomarkers guides diagnosis.
While there’s no definitive cure, intensive speech‑language therapy, management of secondary motor or swallowing issues, and vigilant monitoring for Parkinson‑like syndrome features can preserve quality of life. Staying informed about research, especially trials targeting tau, empowers patients and families to make proactive choices.
If you suspect PAOS in yourself or a loved one, don’t wait. Reach out to a neurologist or speech‑language pathologist today. Early intervention can keep conversations flowing longer, and together we can navigate this journey with compassion, knowledge, and hope.

















Leave a Reply
You must be logged in to post a comment.