Hey there! If you’ve ever felt that strange, nagging pain in your throat, ear, or jaw and wondered whether it’s something serious or just a random ache, you’re not alone. Two conditions—Eagle Syndrome and Ernest Syndrome—often get tangled up in the same conversation because they share a lot of symptoms. The good news? Knowing the key differences can steer you straight to the right doctor, the right test, and the right relief.
Let’s cut through the confusion together. I’ll walk you through the anatomy, the hallmark signs, how doctors figure out which syndrome you have, and what treatment options actually work. Think of this as a friendly chat over coffee, with a dash of science to keep things solid.
Why They Confuse
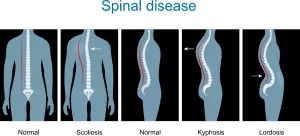
Both Eagle and Ernest syndromes belong to a family of head‑and‑neck problems that cause head and neck pain and can make everyday activities like swallowing or turning your head feel like a mini‑battle. Because they both involve structures near the jaw and throat, patients (and sometimes even doctors) can mistake one for the other. In many cases, people first get labeled with “TMJ disorder” or “sinus pain” before the real cause is uncovered.
Imagine trying to solve a mystery with two suspects who look almost identical. That’s why a careful look at the symptoms and a targeted exam are crucial. Below you’ll see exactly what each “suspect” brings to the table.
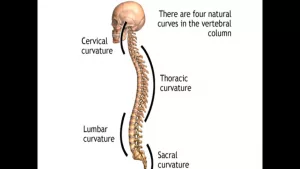
Anatomy Basics
Understanding where the pain is coming from makes a huge difference. Here’s a quick snapshot:
| Feature | Eagle Syndrome | Ernest Syndrome |
|---|---|---|
| Primary structure | Elongated styloid process (>30 mm) or calcified stylohyoid ligament | Stylomandibular ligament (SML) irritation/tendinosis |
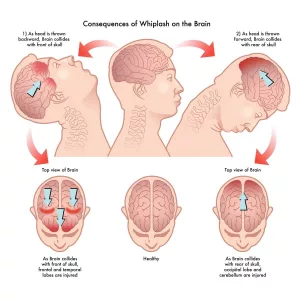
| Typical cause | Congenital elongation, trauma, chronic ossification | Ligament injury from whiplash, dental work, excessive yawning |
| Affected nerves | Glossopharyngeal, vagus, carotid plexus | Auriculotemporal & mandibular nerves |
| Key imaging | Pan‑or‑CT showing long styloid bone | Palpation + local‑anesthetic block (no bone abnormality) |
These differences are reflected in the way the pain travels and what doctors look for on scans. In fact, Healthline explains that an elongated styloid is the hallmark of Eagle, while Ernest hinges on ligament inflammation.
Core Symptoms
Eagle Syndrome Symptoms
People with Eagle often describe a feeling of something “stuck” in the throat, especially when they turn their head to one side. Common clues include:
- Sharp throat pain that radiates toward the ear.
- Difficulty swallowing (dysphagia) or a constant sensation of a lump.
- Pain that worsens when rotating the head.
- Ear fullness or tinnitus, sometimes mimicking an ear infection.
- In severe, rare cases, vascular symptoms like fleeting dizzy spells (because the elongated bone can press on nearby arteries).
Ernest Syndrome Symptoms
Ernest’s pain tends to stay closer to the jaw and the area behind the ear, where the stylomandibular ligament attaches. Look for these signs:
- Localized tenderness at the back corner of the lower jaw, right below the ear.
- Jaw ache that may worsen with chewing or wide‑mouth yawning.
- Ear pressure or mild tinnitus, often confused with TMJ disorders.
- Referred pain that can travel to lower teeth, cheekbones, temples, or even the eye.
- Clicking, locking, or limited opening of the jaw.
Because the symptom sets overlap, a quick self‑check can help you see which pattern matches you best. If the pain shoots up your throat when you turn your head, Eagle is more likely. If the pain is stubbornly anchored behind the ear and follows the jaw, think Ernest.
How to Diagnose
Clinical Examination
Doctors start with a hands‑on exam. For Eagle, they may feel a hard bump in the tonsillar fossa and reproduce pain by pressing on the styloid area. For Ernest, they’ll gently press along the stylomandibular ligament’s path; a sharp “ouch” that eases after a local anesthetic block is a big clue.
Imaging & Tests
Imaging is the gold standard for Eagle. A simple panoramic X‑ray or a CT scan will show a styloid longer than 30 mm. A PubMed case series notes that radiographic confirmation is essential before any surgical plan.
Ernest doesn’t usually show up on X‑rays because it’s a soft‑tissue problem. Diagnosis relies on:
- Palpation of the ligament insertion.
- Symptom relief after a diagnostic anesthetic injection.
- In some research settings, MRI can spotlight inflammation, but it’s not routine.
When to Order Which Test?
Think of it like a decision tree: If you have throat pain that flares with head rotation, ask for a CT. If the pain is isolated to the jaw‑ear junction and improves after a local block, imaging may not be necessary—focus on the clinical exam.
Treatment Paths
Eagle Syndrome Management
Most patients start with conservative care:
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) for pain.
- Heat or cold packs and gentle neck stretches.
- Short courses of steroids or local injections for severe inflammation.
If symptoms persist, surgery is the definitive fix. A styloidectomy (removing the elongated bone) or a partial resection often brings rapid relief. According to the Healthline article, most patients feel better within weeks after a well‑planned operation.
Ernest Syndrome Management
Because Ernest is a ligament issue, the treatment toolbox is a bit different:
- Physical therapy focused on neck and jaw mobility.
- NSAIDs or muscle relaxants to calm inflammation.
- Targeted corticosteroid or prolotherapy injections at the ligament site.
- For stubborn cases, minimally invasive radiofrequency ablation or a surgical release of the stylomandibular ligament can be considered.
A systematic review from 2020 found that corticosteroid injections provided significant pain relief for the majority of patients, while surgical release was reserved for those who didn’t respond after several months of conservative care.
Choosing the Right Path – Patient‑Centric Tips
Here’s a quick cheat sheet to help you (or your doctor) decide:
- Imaging shows a long styloid? – Think Eagle, consider surgical evaluation.
- Palpation points to the stylomandibular ligament and injections help? – Ernest is likely.
- Symptoms include vascular issues (dizziness, vision changes)? – Eagle, because the bone can press on carotid structures.
- Pain spikes after a whiplash or dental procedure? – Ernest, as ligament trauma is common after those events.
Expert Insights & Real‑World Stories
Dr. Ross Hauser, MD, a long‑time pain specialist, often calls Ernest “the missing diagnosis” for patients who keep getting “TMJ treatment” without relief. He wrote, “When we finally locate the stylomandibular ligament irritation, a single injection can change a patient’s life” (CaringMedical).
Case 1 – The Whiplash Survivor
A 32‑year‑old office worker was in a rear‑end collision. He developed constant jaw pain that didn’t improve with splints or orthodontic work. A careful palpation revealed tenderness at the stylomandibular ligament. A diagnostic block erased the pain for 48 hours, confirming Ernest. After a series of prolotherapy injections, his jaw returned to normal and he could finally eat popcorn again.
Case 2 – The Teacher with a “Stuck” Throat
A 45‑year‑old elementary teacher kept complaining of a feeling that something was lodged in her throat, especially when she turned her head to face the classroom. An ENT ordered a CT scan that showed a 38 mm styloid process. She underwent a minimally invasive styloidectomy and was symptom‑free within three weeks. She told us, “I can finally say ‘good morning’ without wincing.”
These stories illustrate why accurate diagnosis matters: the right label leads to the right treatment, and the wrong one can send you on a costly, frustrating odyssey of tests and medications.
Bottom Line – How to Tell Them Apart
To sum it up in everyday language:
- Location of pain – Eagle = throat & ear when you turn the head; Ernest = jaw/ear area at the back of the lower jaw.
- What the doctor feels – Eagle = hard bone bump; Ernest = tender ligament.
- Imaging needs – Eagle requires a scan; Ernest is often diagnosed by exam and a simple injection.
- Typical treatments – Eagle = possible surgery to trim the bone; Ernest = physical therapy, injections, and occasionally a minor release surgery.
If any of the symptoms above sound familiar, don’t just chalk it up to “stress” or “bad posture.” Schedule an appointment with an oral‑maxillofacial surgeon or an ENT specialist—ideally someone who’s comfortable with facial pain syndromes. Bring this guide with you; it will help you ask the right questions and feel more confident during the exam.
Take the Next Step
Feeling a little less uncertain? Good! Knowledge is the first step toward relief. Download a printable version of this comparison chart (or copy the table above) and keep it handy for your next doctor’s visit. And remember, you’re not alone—many people walk this path, and the right diagnosis can change everything.
What’s your experience with head‑and‑neck pain? Have you been told it’s TMJ, then later discovered it was Eagle or Ernest? Drop a comment below, share your story, and let’s help each other navigate this confusing terrain. If you have any lingering questions, feel free to ask—I’m here to help!




















Leave a Reply
You must be logged in to post a comment.