Yes – you can have cirrhosis and still see “normal” liver function test results. It feels like the medical world is playing a trick on you, especially when you’ve been told to watch your alcohol intake or manage hepatitis, yet your blood work looks perfectly fine.
Why does this happen? Because the liver is a champion of compensation. It can keep doing its job even when a lot of its tissue is scar‑red. This article unpacks the mystery, shows you which tests actually matter, and gives you a toolbox so you never get caught off‑guard by a “normal” result.
Why Tests Appear Normal
What Does “Compensated Cirrhosis” Mean?
Think of the liver as a factory with many assembly lines. In compensated cirrhosis, enough of those lines are still running smoothly that the factory can meet the city’s demand—even though half the building is under construction. The body’s “backup generators” (extra blood flow, extra protein production) keep things humming, so the usual blood tests (ALT, AST, ALP, GGT) may stay inside the normal range.
How the Liver’s Reserve Masks Injury
The liver has an enormous functional reserve – estimates suggest you can lose up to 70 % of healthy tissue before you feel any symptoms. When that reserve is still active, enzymes that leak from damaged cells (the “injury markers”) don’t rise enough to cross the laboratory’s cut‑off.
Numbers That Tell the Story
Studies show that roughly one‑third of patients with advanced cirrhosis have normal ALT and AST levels (Sharma 2021). Healthline reported a similar finding in 2025, noting that compensated disease often hides behind “normal” labs.
Mini‑Case Study
Mike, 55, drinks socially and was diagnosed with alcohol‑related cirrhosis three years ago. Every six months his ALT and AST hover around 25 U/L – perfectly normal. It wasn’t until an ultrasound picked up early nodular changes that his doctor started a surveillance program. Mike’s story illustrates why “normal” doesn’t always equal “safe”.
Tests vs. Injury Markers
Not all liver‑related blood work measures the same thing. Below is a quick glance at what each test really tells you.
| Test | What It Measures | Normal Does … | Can Miss … |
|---|---|---|---|
| ALT / AST | Hepatocyte injury | May be normal in compensated cirrhosis | Advanced fibrosis or scarring |
| ALP / GGT | Biliary (cholestasis) injury | Normal if bile flow is okay | Early intra‑hepatic cholestasis |
| Albumin | Synthetic function | Normal early, drops later | Late‑stage decompensation |
| PT / INR | Clotting factor production | Normal early, rises with severe disease | Early fibrosis (often missed) |
| Bilirubin | Excretory function | Normal until late disease | Early cirrhosis |
According to the American Academy of Family Physicians, “normal” aminotransferases do not guarantee a healthy liver; they merely suggest that massive cell death isn’t occurring at the moment (A‑AFP 1999).
Why ALT/AST Aren’t the Whole Story
ALT is mostly liver‑specific, while AST lives in muscles, heart, and even the brain. A normal ALT can be reassuring, but if AST is sneaking up – especially in an alcoholic patient – the AST/ALT ratio can hint at underlying damage. In many cirrhosis cases, both stay quiet.
The Role of Synthetic Tests
Albumin, bilirubin, and PT/INR are the real “function” markers. When these drift out of range, they signal that the liver’s “factory output” is faltering. Unfortunately, they often change only after the scar tissue has already built up.
Child‑Turcotte‑Pugh Snapshot
These three synthetic tests (plus clinical signs of ascites and encephalopathy) are part of the Child‑Turcotte‑Pugh (CTP) score, the gold standard for staging cirrhosis. A CTP‑A score can still accompany perfectly normal ALT/AST – proof that function and injury are two different movies.
Diagnostic Toolbox When Normal
When your labs look innocent, you need other tools to unmask hidden disease.
Imaging: From Ultrasound to FibroScan
Standard abdominal ultrasound can spot nodules, splenomegaly, or signs of portal hypertension. If you want a more precise picture, transient elastography (FibroScan) measures liver stiffness – values > 12 kPa often indicate cirrhosis, even if bloodwork is pristine.
Serum Biomarkers: APRI & FIB‑4
The AST‑to‑Platelet Ratio Index (APRI) and the Fibrosis‑4 (FIB‑4) score combine simple labs into a risk calculator. According to a 2021 Australian prescribing guide, an APRI > 1.5 predicts cirrhosis with solid specificity (Gupta & Walker 2021).
Quick APRI Reference
| APRI Score | Interpretation |
|---|---|
| < 0.5 | Low risk of significant fibrosis |
| 0.5 – 1.5 | Indeterminate, consider further testing |
| > 1.5 | High risk of cirrhosis |
Complete Blood Count: The Platelet Clue
Thrombocytopenia (platelet count < 150 × 10⁹/L) appears in about 70 % of cirrhosis patients, even when LFTs look fine (VA Hepatitis 2014). Low platelets are a red flag that the spleen is getting crowded because of portal hypertension.
Liver Biopsy: The Last Resort
If imaging and biomarkers disagree, a percutaneous liver biopsy can give a definitive answer. It’s invasive, so doctors reserve it for puzzling cases where the treatment plan hinges on certainty.
Risks of Relying on Normal
False Reassurance
Imagine you’re driving with a broken brake light but you keep checking the speedometer – it reads perfectly fine, so you keep going faster. Normal liver labs can give that same false sense of security, delaying referral and allowing disease to progress silently.
Common Pitfalls
• Obesity can modestly raise ALT, masking a normal‑ish value.
• Some ethnic groups naturally have slightly higher baseline aminotransferases, so “normal” cut‑offs might be misleading (A‑AFP 1999).
• Alcoholic liver disease often shows normal ALT but an elevated AST/ALT ratio (> 2).
When to Call a Specialist
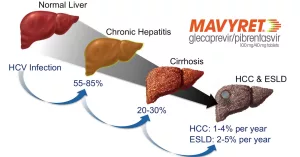
- Any history of chronic hepatitis B or C.
- Long‑standing heavy alcohol use (≥ 30 g/day for men, ≥ 20 g/day for women).
- Persistent risk factors plus an ultrasound showing nodularity.
- Unexplained thrombocytopenia or splenomegaly.
Primary‑Care Checklist
- Review risk factors (viral hepatitis, alcohol, NAFLD).
- Check LFTs + albumin/PT/INR.
- If labs normal but risk present → order abdominal ultrasound.
- Calculate APRI/FIB‑4; if high, refer to hepatology.
- Document patient education and follow‑up plan.
Real‑World Experiences
Story #1: “The Silent Test”
Laura, 42, came for her annual check‑up. She felt fine, had no alcohol habit, but a family member had hepatitis C. Her ALT/AST were 22 U/L and 19 U/L – textbook normal. Her doctor, remembering that family history raises stakes, ordered a FibroScan. The stiffness reading was 13 kPa, confirming early cirrhosis. Laura now follows a low‑sugar diet, avoids alcohol, and gets six‑monthly scans. She says, “If my doctor hadn’t dug deeper, I’d still be clueless.”
Story #2: “The Missed Warning”
James, 60, had a history of heavy drinking. His routine labs were always “normal” – his doctor reassured him that the liver was fine. Two years later he presented with ascites and jaundice; imaging revealed decompensated cirrhosis. He wishes he had asked, “What should I watch for if my tests look okay?”
Expert Insight
Dr. Maya Patel, board‑certified hepatologist, explains: “Normal aminotransferases are a comforting sight, but they’re only a piece of the puzzle. We always pair them with imaging and non‑invasive scores. The moment you have risk factors, you start looking beyond the numbers.”
Bottom Line & Action
Here’s the takeaway you can remember on your next doctor’s visit:
- Normal liver enzymes ≠ a healthy liver. The organ can compensate, especially in compensated cirrhosis.
- Look at function tests (albumin, PT/INR, bilirubin) and platelet count. They often reveal the hidden strain.
- Ask for an ultrasound or FibroScan** if you have any risk factor, even when labs look pristine.
- Use simple scores (APRI, FIB‑4). They turn ordinary labs into powerful predictors.
Don’t let a “normal” result lull you into false safety. Talk to your clinician, request the additional screening tools, and keep an eye on your lifestyle choices. Your liver may be quietly working overtime – give it the support it deserves.
Got questions or personal experiences about liver testing? Share them in the comments below – we’re all learning together. And if you’d like a printable “Cirrhosis‑Screening Checklist,” click here to download. Take care of your liver; it’s the only one you’ve got.






















Leave a Reply
You must be logged in to post a comment.