Did you know that up to 90 % of lung‑cancer cases are linked to preventable exposures, yet many people still think they’re safe if they never smoked? Below you’ll get the straight‑forward facts on the biggest risk factors, how early detection works, and practical steps you can take today to protect yourself.
Core Risk Factors
When we talk about lung cancer risks, the first thing that comes to mind is smoking. And for good reason—cigarette smoke is a toxic cocktail of more than 7,000 chemicals, at least 70 of which are known carcinogens. According to the CDC, smokers are 15 to 30 times more likely to develop lung cancer than non‑smokers. The risk isn’t just “yes or no”; it climbs with every pack‑year you rack up, whether you light a “light” cigarette or a full‑strength one.
But smoking isn’t the sole player. Here are the other culprits that quietly add to your lung cancer risks:
Second‑Hand Smoke
If you think only the smoker gets hurt, think again. Breathing in other people’s smoke, whether at home, work, or a smoky bar, raises your risk by roughly 20 %. It’s the third‑most common cause of lung cancer in the United States. So even if you never light up, staying in a smoke‑filled environment can still put you on the radar.
Radon Exposure
Radon is an invisible, odorless gas that seeps from soil and rock into our homes. The EPA estimates that radon causes about 21,000 lung‑cancer deaths each year, making it the second‑leading cause after smoking. The danger spikes for smokers, but even a never‑smoker isn’t immune—about 10 % of radon‑related deaths occur in people who never smoked.
Occupational & Environmental Toxins
Asbestos, silica, diesel exhaust, arsenic, and certain forms of chromium are all known lung carcinogens. Workers in construction, shipyards, or factories that handle these materials face a heightened risk, especially if they also smoke. The combination of tobacco and occupational exposure can multiply the danger far beyond the sum of each factor alone.
Family History & Genetics
Having a close relative with lung cancer can double your odds. While genetics alone don’t guarantee you’ll develop the disease, they can make you more susceptible to the harms of smoking, radon, or occupational exposures.
Medical & Lifestyle Factors
Previous chest radiation therapy, HIV infection, chronic lung diseases like COPD, and even certain dietary supplements (beta‑carotene, when taken by smokers) can tip the scales. Air pollution in heavily industrialized areas also adds a subtle but real layer of risk.
Real‑World Numbers
Understanding risk in plain numbers helps you see where you stand.
| Risk Factor | Relative Increase | Typical Exposure |
|---|---|---|
| Current Smoking | ≈20× higher | ≥1 pack/day for 20+ years |
| Second‑hand Smoke | ~1.2× higher | Living with a smoker |
| Radon (high indoor levels) | ~2× higher | ≥4 pCi/L at home |
| Asbestos Exposure | ~5× higher | Construction/shipyard work |
| Family History | ~2× higher | First‑degree relative |
These figures are averages; individual risk can vary widely based on age, gender, and how many of these factors stack up in your life.
There are online calculators that let you input your smoking history, radon exposure, and occupational background to estimate a personal risk score. They’re useful conversation starters with your doctor, especially when deciding whether you qualify for a screening program.
Early Detection
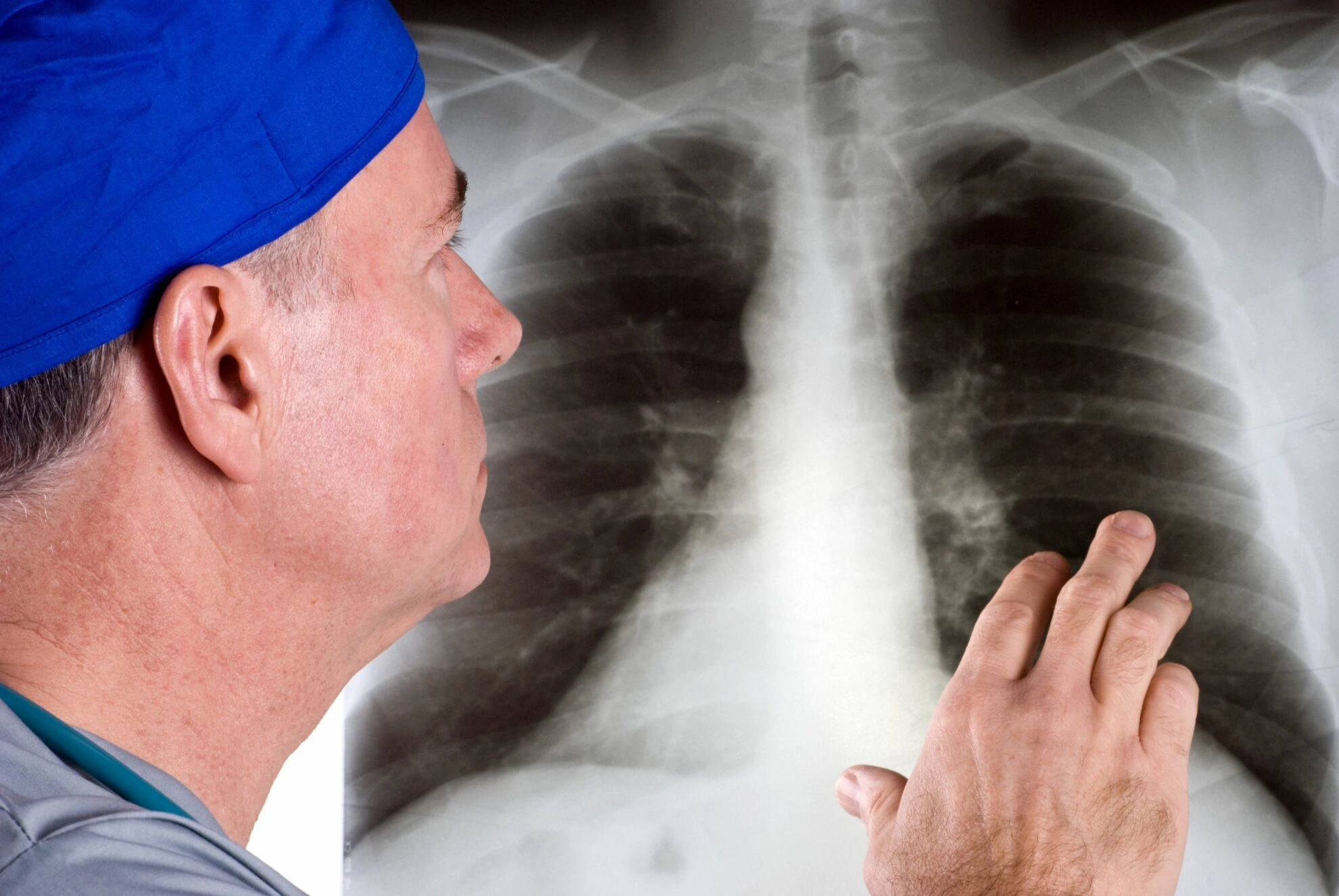
Finding lung cancer early can be a game‑changer. The good news is that a low‑dose computed tomography (CT) scan—a simple, quick lung cancer screening test—has been shown to cut mortality by about 20 % in high‑risk groups. Here’s how to decide if you belong in that group.
Who Should Get Screened?
The U.S. Preventive Services Task Force recommends annual screening for adults aged 55‑80 who have a 30‑pack‑year smoking history and either currently smoke or quit within the past 15 years. This is the classic definition of a lung screening program. If you fit the bill, talk to your primary‑care provider about setting up a low‑dose CT.
What the Test Involves
A low‑dose CT takes pictures of your lungs in just a few minutes. The radiation dose is tiny—about one‑tenth of a standard chest CT—so the test itself isn’t a major source of risk. However, false positives can happen, leading to extra scans or biopsies that may cause anxiety. That’s why it’s essential to weigh early lung cancer detection benefits against potential harms.
Benefits of Screening
Screening catches cancers when they’re still small and more treatable. Studies show that people diagnosed through low‑dose CT are far more likely to be eligible for surgery—a curative option—than those whose tumors are found after symptoms appear. In short, the cancer screening benefits include not just longer life, but a better quality of life because treatment can be less aggressive.
Potential Harms
Over‑diagnosis—finding tumors that would never cause symptoms—can lead to unnecessary procedures. Also, repeated CT scans add a small amount of radiation exposure over time. That’s why doctors only recommend screening for people whose risk is high enough to outweigh these downsides.
Personal Risk Reduction
Even if you’re not yet eligible for screening, you can still lower your lung cancer risks today.
Quit Smoking—The Most Powerful Move
Quitting is the single most effective thing you can do. Your risk drops by about half after ten years without cigarettes and keeps climbing down, approaching that of never‑smokers after 20–25 years. If you’ve tried before and slipped, that’s okay—each attempt gets you closer. Resources like quitlines, mobile apps, and nicotine‑replacement therapy can make the journey smoother.
For a deeper dive into how quitting affects risk, check out our smoking and lung cancer guide.
Test & Mitigate Radon
Radon kits are cheap and easy—just place a detector in your basement for a few days and send it to a lab. If levels are above 4 pCi/L, professional contractors can seal cracks and improve ventilation, cutting radon‑related risk by up to 80 %.
Protect Yourself at Work
If you work with asbestos, silica, or other known carcinogens, make sure your employer follows OSHA safety standards: proper protective equipment, regular air monitoring, and clear decontamination procedures.
Adopt a Lung‑Friendly Lifestyle
Exercise, a diet rich in fruits and vegetables, and staying hydrated all contribute to overall lung health. While no food can “cure” cancer, antioxidants help neutralize some of the damage caused by inhaled toxins.
Stay on Top of Medical Check‑Ups
Even if you feel fine, an annual physical can flag early warning signs—persistent cough, unexplained weight loss, or shortness of breath. Bring up any family history or occupational exposures; your doctor may recommend earlier or more frequent screening.
Key Takeaways
Let’s boil it down to the essentials:
- Smoking remains the biggest modifiable risk. Quitting, even later in life, still cuts your chances dramatically.
- Second‑hand smoke and radon are silent threats. Test your home for radon and avoid smoke‑filled environments whenever possible.
- Occupational exposures add a significant layer of risk. Use protective equipment and advocate for safe workplace practices.
- Early detection saves lives. If you meet the criteria for a lung screening program, talk to your doctor about a low‑dose CT.
- Your family history matters. Share any cancer diagnoses with your healthcare team so they can tailor your screening plan.
Take a moment right now: check your smoking history, see if you’ve tested your home for radon, and schedule a chat with your doctor about whether you qualify for lung‑cancer screening. Small steps add up, and together they turn a scary statistic into a story of empowerment.
We’d love to hear what actions you’re planning to take. If you have questions, feel free to reach out—your health journey is personal, and you don’t have to walk it alone.



















Leave a Reply
You must be logged in to post a comment.