
Why All the Confusion?
Okay, can we just be honest for a sec? Modern health talk is a mess. News headlines shout “opioid crisis” while doctors drop words like “infusion therapy.” It’s enough to make your brain tangle. And in the middle of all this chaos—bam—here’s ketamine, popping up as a pain option. Tons of you might be thinking: Is ketamine an opioid? I get it. It shows up in the same conversations. Sometimes even in the same hospital rooms. But the answer? Not as simple as “yes” or “no”… but mostly, pretty solidly “no.”
Let’s unpack this together—like a chat with a friend over coffee (with a shot of science).
Same Pain, Different Pathway
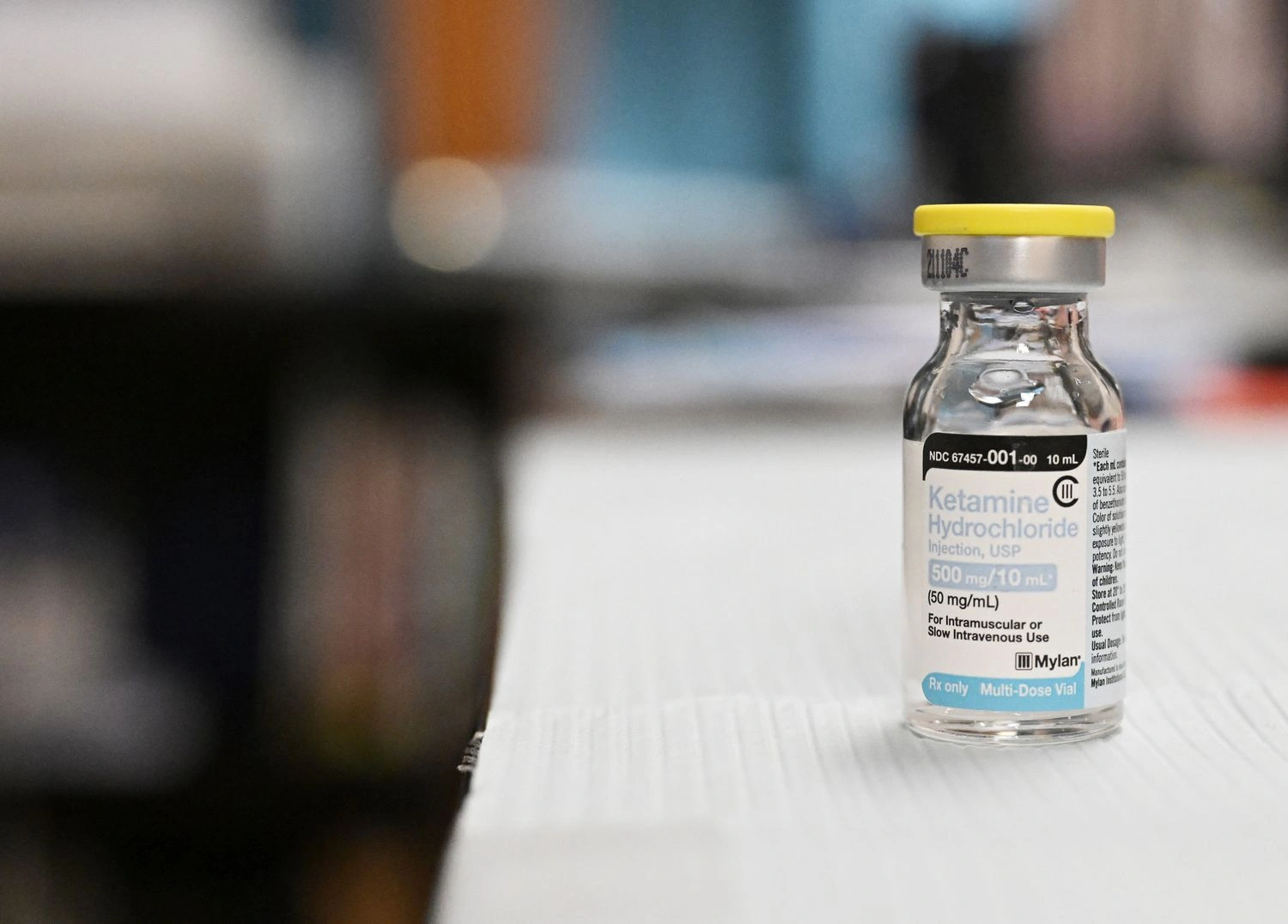
So, why do folks mix up ketamine with opioids in the first place? Easy—both are used to treat tough pain. Say you have a killer injury, or chronic pain that just won’t quit—an ER doc or pain doc might reach for ketamine if the usual opioid suspects aren’t working (or if you’re just not keen on the sticky side of narcotics). Maybe you’ve heard stories about it being a go-to in emergencies, or whispered about as the “backup for morphine.” It’s all true…sorta.
But—and it’s a big but—the way ketamine works in your body is basically a different universe. Ketamine blocks something called NMDA receptors in the brain (science talk, I know, but stick with me), while opioids like morphine or oxy stick to opioid receptors. Think of it like two completely different locks, and neither has the other’s key. You can read more on what is ketamine used for medically if you’re curious about the medical side.
But Wait, Didn’t Researchers Find Some Connection?
Great catch—because, yeah, things aren’t always 100% simple. There was that wild Stanford study with rats (yes, rats… but that’s science for you). Turns out, when they blocked opioid pathways in male rats, ketamine sort of lost its magic for them. For female rats? Not so much—the effect stuck around. Isn’t biology weird? (Humans are even messier.)research on ketamine and opioid interaction Sure, ketamine can flirt with some of the same brain paths as opioids, but that doesn’t make it one.
Table Time: How Ketamine and Opioids Compare
| How it Works | Ketamine | Opioids |
|---|---|---|
| Brain Receptor Target | NMDA, some glutamate | Opioid receptors (mu, kappa, delta) |
| Main Use | Anesthesia, hard-to-treat pain, depression | Pain relief, cough suppression (sometimes), anesthesia |
| Dependency/Addiction Risk | Possible, but lower; mostly psychological | High; physical + psychological |
| Notorious Side Effects | Dissociation (“out of body”), hallucinations, raised heart rate | Drowsiness, constipation, overdose (respiratory depression) |
| Reputation | Medical, “club drug,” misunderstood, newsy | Essential medicine & crisis headline |
So, next time someone drops “is ketamine an opioid” in your group chat, you can be the smart one—”Nope, totally different locks and keys.”
The Real-World Side: When Docs Choose Ketamine
Maybe you’re thinking, “Okay, got it… so why would my doctor even pick ketamine if it isn’t an opioid?”
Here’s the thing: sometimes, opioids don’t work, or you just don’t want to risk all the garbage side effects. Or maybe you’ve been burned by opioids before (show of hands?). Ketamine steps in as the alternative, especially in tough pain scenarios—like battlefields, wild ER nights, or that neighbor’s dad who swears it was a “game-changer” for his chronic nerve pain.
Actually, quick story—my friend’s mom had back pain so bad she said she’d have “traded in her own dog for relief.” (We laughed…but I think she meant it.) When the usual stuff flopped, they tried low-dose ketamine under hospital watch. Within days, she was back on her feet, cautiously optimistic and way less grumpy. (Bonus: the dog got to stay.)
Check out What is ketamine used for if you want to see more weird and wonderful real medical uses—hint: it helps with more than pain.
So… Is Ketamine as Good as Morphine?
Funny enough, some recent research put ketamine up against morphine for emergency pain and… they tied. Non-inferior, as they say in med labs. Pretty wild, right? That means if you’re writhing in pain, ketamine could give you just as much relief as the “big O”…and often without slowing down your breathing or knocking you out cold.
(Of course, the details can get complicated—doses, side effects, what the rest of your body’s doing that day. Medicine is tricky.) There’s a study showing that in some cases, ketamine even boosted blood pressure a bit, which is handy if you’re in shock, not so great if you’ve already got a sky-high heart rateresearch comparing ketamine and morphine. But overall: new options matter, especially in a world overwhelmed by opioid risks.
When Ketamine Makes Sense (And When It Doesn’t)
Let’s keep it real: ketamine isn’t fairy dust or some risk-free hack. Used right, it’s ridiculously helpful for:
- Severe, opioid-resistant pain (like certain nerve issues)
- Painful cancer situations, when nothing else helps
- Emergency anesthesia (think battlefield, serious car crashes, surgery)
- Even mood stuff—think “treatment-resistant depression”
But it’s not for headaches, sprained ankles, or DIY use at home. When it comes to chronic pain (after the acute emergency passes), guidelines get pretty strict. In supervised medical settings, ketamine’s magic shines. On your own? Not so much—it’s not a home remedy.
The Messy Side: Dependency, Safety, and Media Drama
Let’s get honest about the fears, too. Maybe you heard about Matthew Perry’s tragic end or the headlines linking ketamine to party scenes (ugh, “Special K” is not a healthy smoothie flavor).
So, does that mean you’ll get addicted, or become the next news story? Not really—at least, not if small doses are used as prescribed and supervised. Your odds of classic opioid-style withdrawal? Much lower. Still, ketamine isn’t a risk-free ride. (No medicine is, honestly.)
What could happen? Well, if you take way too much, or mix it with other stuff, you could wind up disoriented, hallucinating, or feeling seriously detached (oh hey, “K-hole”). High doses, long term? Potential for bladder problems, memory lapses, and in rare cases, dependency. But physical withdrawal isn’t the main risk—psychological cravings are more likely (especially for folks who get hooked on that floaty “escape reality” feeling).
That’s why your doc or clinic team will keep things tight—low doses, slow increases, and tons of checks. And if you Google stories about unsupervised use—yeah, things can get messy Johns Hopkins on ketamine’s unique risks and benefits.
For the Risk Takers (And the Cautious)
If you’re the type who reads every warning label, ketamine’s for you—but only with proper supervision. If you’re more the “I’ll figure it out myself” type…maybe pump the brakes. Safe use is all about context and expert guidance, not rolling the dice.
Brief Table: Ketamine Pros and Cons
| Pros | Cons / Warnings |
|---|---|
| Works when opioids don’t | Bladder trouble with long use |
| No breathing suppression | Hallucinations (“out of body”) |
| Fast, effective relief | Can raise heart rate / blood pressure |
| Less likely to cause physical dependency | Not for everyone, needs monitoring |
Honestly, ketamine’s reputation is still a jumble—some see a savior, others see a scandal. The best thing? Read up, ask questions, and talk to real humans (docs, nurses, even patients). Or start with articles like what is ketamine used for medically and What is ketamine used for for deeper dives.
Stories That Stick (A Little Mess, a Lot of Hope)
Let’s sprinkle in some real life. Have you noticed how pain, depression, and chronic illness sort of gang up on you when you’re feeling most alone? For me, seeing friends try ketamine after years of dead ends—watching them get a few good days back—feels like watching someone walk through a door they thought was welded shut. It’s not always a miracle, not a cure, and yeah, stuff can go sideways…but when it works, wow. There’s a shift in how they move, talk, even laugh again.
If this is you, or could be you—if you’re the “nothing else worked” person—you’re not crazy for wondering about ketamine. It’s worth asking about.
So, Is Ketamine an Opioid? (And Should You Care?)
Time for the one-line answer: Nope, ketamine is not an opioid. Not chemically, not in how it hooks up with your brain, not in the way it creates dependency. It just gets tossed into that basket because, in the hunt for pain relief, both are in the running. But honestly? We need more tools in the pain toolbox, not fewer—and ketamine’s offering hope for the “that’s my last nerve” crowd.
Here’s where you come in. If you’re wrestling with stubborn pain, or just want to weigh your options (for yourself or someone you love), give your doc a nudge. Ask about ketamine—not because it’s magic, but because you deserve every chance at a bright day. Let’s keep this conversation messy, open, and honest. After all, real answers rarely fit in a simple “yes or no.” But isn’t that what makes life interesting?
So… what do you think about this approach? Would you try ketamine if the “usual” pain plan failed? Or do you have your own story or worry bubbling up? (Seriously—drop me a note, or share in your next doctor visit.) Either way, don’t let confusion or stigma block your shot at relief. We’re in this weird adventure together.

















Leave a Reply
You must be logged in to post a comment.