Old Drug, New Chapters
Let’s start with a scene you might recognize. You’re at the doctor, maybe getting stitches after a kitchen mishap, or you’re waiting for your child’s surgery. The anesthesiologist says, “We’ll use ketamine.” You nod—maybe you’ve heard of it as a “club drug” or read something wild about its use for depression. But honestly, what is ketamine used for medically, really? Why do so many doctors, pain specialists, and even mental health professionals keep talking about it?
Here’s the quick truth: ketamine is a medical chameleon. For decades, it’s been the go-to for anesthesia, short surgeries, and intense pain. These days, though? It’s popping up everywhere from pain clinics to mental health centers. And yes, sometimes it’s even life-changing. We’ll get into all of that—no filter, no fluff, just straight talk, a few stories, and maybe a joke or two along the way. Ready?
How Does Ketamine Really Work?
From the Battlefield to the Operating Room… to Your Local ER
So… let’s time travel. The year is 1970. The Vietnam War is raging, and doctors need a drug that gets wounded soldiers unconscious fast, doesn’t stop breathing, and—this bit is key—is safe even in chaos. Ketamine steps up. It can put you “under” for surgery or deliver enough sedation for resetting a broken arm. Fast forward: it’s still used in hospitals worldwide for those very reasons.
Why? Ketamine is what docs call a “dissociative anesthetic.” In simple terms, it blocks the pain signals but keeps your body pretty stable. You’re not completely “out” like with some other sedatives, so your breathing ticks along naturally. (Yes, this has saved a lot of lives in emergencies.) According to medical research on ketamine’s medical indications, this drug is a top pick for quick procedures, putting people to sleep before surgery, and even for those with tricky breathing issues.
Ketamine vs. Traditional Anesthetics—A Quick Look
| Aspect | Ketamine | Other Anesthetics (e.g., Propofol) |
|---|---|---|
| Onset time | Minutes | Seconds to minutes |
| Muscle relaxation | Minimal | Full |
| Best for | Emergency, short ops | Major, planned surgeries |
| Pain relief effect | Strong, even under low doses | Varies |
| Key risks | Hallucinations | Breathing problems |
Point is, ketamine covers your bases for both pain and fast, safe anesthesia, especially when seconds count. But there’s more to this story…
When Pain Won’t Quit
Could One Infusion Change Life with Chronic Pain?
Let’s get real—chronic pain is a bully. It lurks in your back, zaps your energy, and before you know it, everything feels harder. Maybe you’ve tried muscle relaxants, over-the-counter pills, or even opioids… and they didn’t work. Here’s where ketamine gets interesting. Clinics now use low-dose infusions (not enough for anesthesia, but enough to make a difference) to chase away pain from stubborn conditions like fibromyalgia, nerve pain, or migraines.
Honestly, I was skeptical the first time I heard this. A running buddy of mine, Kate, used to count the hours until her next dose of pain meds after a nasty car accident. She was one of those people who’d tried everything. Her doc tried ketamine—she said it felt like someone had finally turned the pain dial way, way down. For the first time in a year, she made it through a day without wincing at every step. Her words? “It was like my body exhaled.” There’s real science behind that—studies show ketamine works differently than opioids, by dampening certain signals in your brain, rather than just numbing everything (see research on depression & chronic pain relief).
Is Ketamine an Opioid?
This one comes up all the time: Is ketamine an opioid? Quick answer: nope. Ketamine is in its own lane, working mostly on what docs call the “NMDA receptor,” not the opioid receptors. If you want a detailed breakdown (including all the official science), check out Is ketamine an opioid—super clear and kind of eye-opening, even for science nerds.
Because ketamine’s not an opioid, the risk of addiction is lower, and it doesn’t cloud your judgment in the same way. It’s an alternative—sometimes the only one—for pain that laughs at regular meds.
How Do Ketamine Infusions Work?
It’s not like picking up a prescription at the pharmacy. You’ll sit in a clinic, get hooked up to an IV, and a nurse or doctor will monitor you. The dose is way smaller than what’s used for surgery—just enough to “take the edge off” the pain or break the mental rut pain can cause. Afterward, some people feel loopy, maybe even a bit dreamy, but honestly? For many, that’s a small trade-off for a break from pain.
Still, there are rules. Not everyone’s a good candidate. People with certain heart problems, high blood pressure, or a history of substance abuse may need extra precautions. As always, talk openly with your doc—seriously, nothing’s “too obvious” to ask.
From Mood “Holes” to Hope
“I Tried Every Pill… Then Ketamine Turned the Lights Back On”
Depression is weird—sometimes you know exactly why it hits, sometimes it just rolls in out of nowhere, gray and unshakeable. Maybe you’ve tried two, three, even a dozen medications. Nothing sticks. Here’s where ketamine quietly started shocking psychiatrists: even in those “hopeless” cases, it sometimes worked. And often, it kicked in within hours or days, not weeks or months (see Yale’s summary on rapid antidepressant action).
I remember talking to someone named Rob at a community group—a guy who’d cycled through more treatments than I could name. After a series of ketamine infusions (again, low-dose, in a clinic), he told me, “It’s like someone flipped a switch—suddenly, the world had color again.” He was suspicious at first. Maybe you are too.
Here’s the science: ketamine helps certain brain chemicals (like glutamate) rewire connections, especially in areas of the brain scrambled by depression (Harvard Health explains more about this rewiring effect). Is it forever? No—effects last days to a couple weeks. It’s not a magic fix, but sometimes, it’s enough momentum to make therapy actually work. More on this if you browse what is ketamine used for medically, which goes deep into the mental health angle.
Ketamine in Clinic vs. Esketamine at the Pharmacy
There’s a twist—if you’ve heard of “Spravato,” that’s a nasal spray version called esketamine. It’s FDA-approved for treatment-resistant depression, used under close watch at approved clinics. The original (IV) ketamine is still often “off-label”—meaning your doctor uses it for depression, but it’s not the official, government-sanctioned use. Make sense?
This route’s growing fast—insurance, rules, all of it is in flux, so know that it’s a field changing by the month. But for folks who’ve run out of road everywhere else? It’s a big leap of hope.
The Weird (and Wonderful?) Side Effects
Hallucinations, Heart Flutters, and the Infamous “K-Hole”
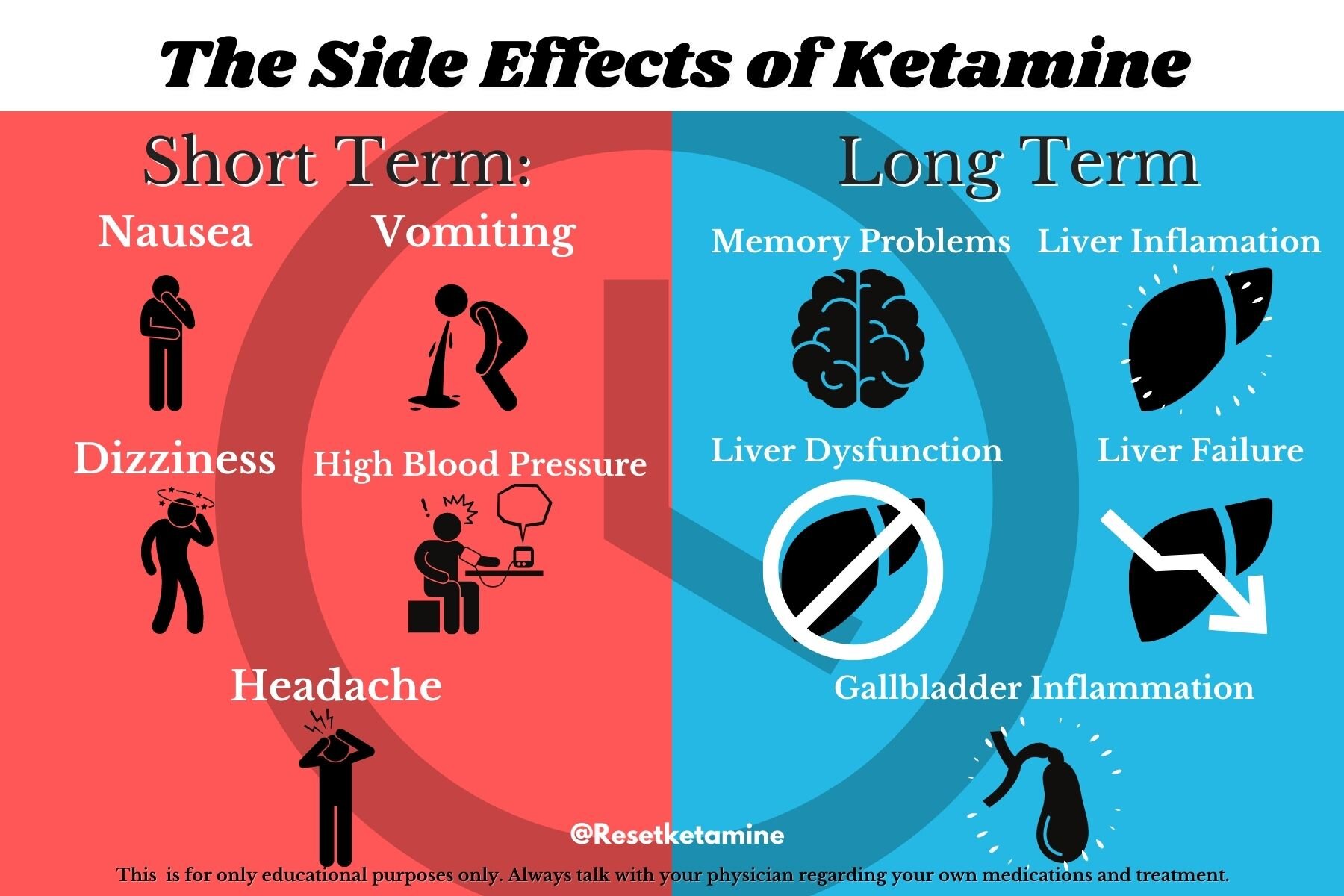
Okay, let’s get awkward. Ketamine is famous (or infamous?) for making people feel weird—sometimes detached, floaty, or even sending them into what’s nicknamed a “K-hole”—like an out-of-body experience. Some call it trippy, some call it terrifying. If you’re being monitored in a clinic, staff are there to help ground you and keep things safe (see safe use guidance from anesthesiologists).
It also does things to your heart—certain folks might get palpitations or higher blood pressure. That’s why you never want to try this at home or without medical help. If you already worry about heart disease or hypertension? It’s another conversation to have before jumping in.
Some side effects fade fast. Some don’t, and there’s also a risk for dependency—though far lower than with opioids, it’s not zero. Some people love how it makes them feel; others say it’s just… too much. That’s why the mental health pieces, like integration therapy along with medical supervision, are gaining traction quickly in clinics and research alike.
The Basics at a Glance
A Table To Recap Ketamine’s Medical Uses
| Medical Use | Typical Setting | Common Dosing | Notes/Stories |
|---|---|---|---|
| Surgical anesthesia | OR, ER, field medicine | High (anesthetist monitored) | Heart surgery, battlefield medics, trauma teams |
| Acute pain management | ER, procedure rooms | Moderate to low dose | Setting bones, treating burn wounds, dental surgery |
| Chronic pain control | Pain clinics | Low-dose IV infusions | Migraines, neuropathy, CRPS, post-surgical pain |
| Treatment-resistant depression | Mental health centers | Smaller, repeated infusions or nasal spray (esketamine) | Often after other antidepressants fail |
You can always find more details on approved and emerging uses over at what is ketamine used for medically—it’s packed with the kind of facts you can bring to your doctor.
Is Ketamine Right for You?
Who Should (and Shouldn’t) Consider It, Really?
Whew—so, maybe you’re curious. Maybe you’re also a little nervous. Both totally fair! Ketamine is serious business. It’s not usually a first stop for anesthesia, pain, or depression, but for some, it’s opened doors nothing else could. The fact that it’s not an opioid, but still helps with agony and despair, is pretty unique—just look at the surge of clinics opening up strictly for ketamine therapy. Still, the best outcomes happen in clinics with specialists who can tailor your dose, spot side effects, and help you integrate the emotional stuff afterward. (Please steer very clear of “DIY” ketamine offers online—this is never something to play with alone!)
You’ll want to avoid ketamine if you have poorly controlled heart disease, a history of psychosis, or if you’re pregnant—basic safety ground rules. And if you want a nerd-level breakdown of how ketamine fits into the pain management world (or the whole “is ketamine an opioid?” thing), here’s the rabbit hole: Is ketamine an opioid.
Looking Forward: Your Takeaway
So—what is ketamine used for medically? It’s a toolbox multitasker: anesthesia for surgeons, quick-acting pain relief for ER doctors, a beacon of hope for folks with chronic pain or depression who’ve felt every other door slam. It’s not for everyone, and it’s definitely not a miracle. But for a growing number of us, it’s… a fresh start. Tired of fighting pain every day? Or feeling stuck in an endless depressive rut? It’s okay to ask about new options—science moves fast, and sometimes so does relief. Even if ketamine isn’t right for you, knowing your choices is powerful.
So talk with your provider. Dig deep into what is ketamine used for medically, jot down questions, and show up ready to advocate for yourself. Recovery is rarely a straight line, but neither is hope. Here’s to your next step out of pain, out of darkness—and into new light, one real conversation at a time.

















Leave a Reply
You must be logged in to post a comment.