Congratulations, you’ve just welcomed a new little one into the world! 🎉 (Okay, I’ll keep the emojis out of the final version, but you get the excitement.) The first few weeks are a whirlwind of diapers, feedings, and tiny‑hand‑holds, but amid the joy it’s easy to miss a sneaky health issue that can sap your energy just when you need it most. That issue is postpartum anemia, and the good news is that the signs are usually clear, the diagnosis is simple, and the treatment works like a charm when you catch it early.
In the next 15‑20 minutes we’ll walk through everything you need to know – from the warning signals your body sends, to why they happen, how doctors confirm the problem, and the best ways to get back to feeling like yourself again. Think of this as a friendly chat over a steaming mug of tea, where I’ll share facts, personal stories, and a few practical tips you can start using today.
Why It Matters
Feeling a little tired after delivery is absolutely normal. Your body just went through a marathon, and now you’ve got a newborn who thinks 2 am is the perfect time for a feed. But when fatigue turns into exhaustion that won’t lift, when your skin looks paler than usual, or when you notice a dip in milk production, something more than “just being a new parent” might be at play.
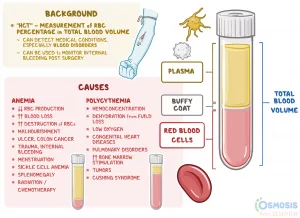
Post‑partum anemia can affect anywhere from 10 % to 80 % of birthing parents depending on where you look. That’s a huge range, but the point is clear: many people experience it. Ignoring the symptoms can lead to prolonged fatigue, mood changes, and even impact your baby’s growth if milk supply drops. Spotting the signs early gives you a quick path to treatment and prevents those downstream complications.
Common Causes
Understanding why postpartum anemia happens helps you see the bigger picture and, more importantly, how to prevent it next time.
Blood Loss During Delivery
Whether you had a vaginal birth or a C‑section, a certain amount of blood loss is expected. On average, a vaginal delivery might lose 500 mL of blood, while a C‑section can reach 1000 mL or more. For most people this is fine, but if the loss is on the higher end, your iron stores can get depleted quickly.
Iron‑Deficiency Before & After Birth
During pregnancy your blood volume expands by about 50 %. If you entered pregnancy with low iron stores, the demand can outpace what you’re eating, leaving you vulnerable right after delivery. Heavy bleeding, multiple births, or a short interval between pregnancies can deepen the deficit.
Other Medical Contributors
Less common, but still worth noting, are deficiencies in vitamin B12 or folate, chronic infections, or inflammatory conditions that interfere with iron absorption. If you have any of these, the anemia might be a bit more stubborn to treat.
Real‑World Snapshot
Meet Maria, a 32‑year‑old first‑time mom who lost about 800 mL of blood during a fairly routine C‑section. By week two she felt “like she’d run a marathon every day,” noticed her skin looking unusually pale, and her baby’s feedings were slower than expected. A quick blood test revealed a hemoglobin of 9.8 g/dL (below the WHO cutoff of 11 g/dL). After a short course of oral iron and a diet tweak, she was back to her sparkling self by week five.
Getting Diagnosis
When you suspect something is off, the first step is a conversation with your OB‑GYN or primary‑care provider. They’ll likely order a few simple blood tests and do a brief physical exam.
Blood Tests You’ll See
- Complete Blood Count (CBC) – Gives you hemoglobin, hematocrit, and the size of your red blood cells.
- Serum Ferritin – Shows how much iron you have stored; it’s the most reliable early marker.
- Transferrin Saturation – Tells you how much iron is actually circulating.
Most labs will flag anemia if hemoglobin falls below 11 g/dL for postpartum individuals. Ferritin under 30 ng/mL usually points toward iron‑deficiency anemia.
Physical Clues Doctors Look For
During the exam they may note pallor of the conjunctiva (the inner eyelids), a rapid heartbeat, or low blood pressure when you stand up. They’ll also ask about milk output and mood—both can be subtly affected.
Your Post‑partum Visit Checklist
- Bring a log of any symptoms you’ve noticed (fatigue level, skin color changes, breathing ease).
- Ask for a repeat CBC if you had anemia during pregnancy.
- Discuss iron‑rich foods and whether you need a supplement.
Treatment Options & Lifestyle Hacks
Now the good part – fixing it! The approach usually starts with iron supplementation and dietary changes, but there are several pathways depending on severity.
Medical Therapies
- Oral Iron Supplements – Most first‑line; take 100–200 mg of elemental iron daily, preferably with vitamin C (a glass of orange juice) to boost absorption.
- IV Iron – For those who can’t tolerate pills or need a rapid boost (e.g., severe blood loss). It can raise hemoglobin within weeks.
- Blood Transfusion – Rare, reserved for life‑threatening anemia or when hemoglobin drops below 7 g/dL.
Nutrition That Boosts Iron Fast
Iron comes in two forms: heme (from animal sources) and non‑heme (plant sources). Heme iron is absorbed about 15‑35 % better, so include at least one animal source daily if you tolerate it.
Sample 3‑Day Iron‑Boost Menu
| Meal | Iron‑Rich Options |
|---|---|
| Breakfast | Fortified oatmeal topped with sliced strawberries and a glass of orange juice |
| Lunch | Spinach and quinoa salad with grilled chicken, pumpkin seeds, and a lemon‑tahini dressing |
| Dinner | Stir‑fried beef strips with bell peppers, broccoli, and brown rice |
| Snack | Roasted chickpeas or a handful of dried apricots |
Pair iron‑rich foods with vitamin C (citrus, bell peppers, tomatoes) and steer clear of coffee, tea, or calcium‑heavy foods around the supplement – they can block absorption.
Managing Side Effects & Staying Consistent
Iron pills can be a bit harsh on the stomach. Try taking them with a small snack, staying hydrated, and splitting the dose if needed. If constipation crops up, add soluble fiber (like oats) and plenty of water.
When to Call Your Provider
- If fatigue persists after 4 weeks of iron therapy.
- If you notice worsening pallor or shortness of breath.
- If your baby’s weight gain slows and you suspect low milk supply.
Prevention: Keep Your Iron Reservoir Filled
Best to avoid the problem before it starts. Here are simple, proactive steps you can weave into your pregnancy and postpartum routine.
Prenatal Iron Optimization
During the second trimester, most doctors recommend 30 mg of elemental iron daily if ferritin is low. Even if your levels are okay, a prenatal vitamin with iron is a safe baseline.
Post‑Delivery Blood‑Loss Monitoring
Don’t be shy about asking your care team how much blood you lost and whether a follow‑up hemoglobin check is needed. A quick test 24 hours after delivery can catch a dip before you feel it.
Diet & Lifestyle After Birth
Keep iron on your plate: red meat, poultry, beans, lentils, tofu, dark leafy greens, and fortified cereals. A daily glass of citrus juice does wonders for absorption. And remember, moderate tea or coffee is fine – just enjoy them an hour apart from your iron supplement.
Printable Iron Tracker
Consider downloading a simple “Post‑partum Iron Tracker” (you can easily create one in a spreadsheet) to record daily supplement intake, meals, and how you feel. Seeing progress on paper can be a real morale boost!
Bottom Line: Take Action Today
Post‑partum anemia is common, but it’s not a fate you have to accept. By staying alert to the hallmark signs – pale skin, lingering fatigue, shortness of breath, dizziness, or a dip in milk supply – you give yourself a fast lane to diagnosis and treatment. A quick CBC, a short course of iron (or IV if needed), and a handful of iron‑rich meals can have you back to chasing after your baby with energy and joy within weeks.
If any of the symptoms above sound familiar, don’t wait for “new‑parent exhaustion” to become your new normal. Talk to your provider, grab that blood test, and give your body the iron it deserves. Your future self (and your little one) will thank you.
Got a story about how you tackled postpartum anemia, or a tip that helped you feel better? Share it in the comments – we’re all in this together, and your experience might be the piece of advice another new parent needs.




















Leave a Reply
You must be logged in to post a comment.