Short answer: THC might calm some of the jittery symptoms that come with an over‑active thyroid, but it doesn’t “fix” the hormone problem. The research is thin, the risks are real, and you should always loop in a doctor before lighting up.
Why keep reading? Because you deserve clear, friendly answers that respect your health journey. Below you’ll find the good, the not‑so‑good, and practical steps you can take if you’re curious about THC and hyperthyroidism.
Quick Look Summary
- Potential benefits: anxiety relief, better sleep, slight short‑term dip in thyroid hormones.
- Key risks: possible worsening of thyroid‑eye disease, psycho‑active side effects, tolerance over time.
- Bottom line: Use only under medical supervision; consider non‑psychoactive options like CBD or standard medication first.
According to a 2025 Healthline review, the evidence for THC helping hyperthyroidism is limited and mixed.
THC Meets the Thyroid
The Endocannabinoid System and Thyroid Tissue
Our bodies have an internal network called the endocannabinoid system (ECS). It’s like a backstage crew that keeps everything running smoothly. Researchers have found cannabinoid receptors (CB1 and CB2) right inside thyroid cells. When THC binds to those receptors, it can nudge hormone release—but the exact choreography is still a mystery.
What the Studies Tell Us
Human data are sparse, but a few key pieces stand out:
- Short‑term use: A handful of acute studies report a modest, temporary drop in T3/T4 after a single THC dose (Healthline, 2025).
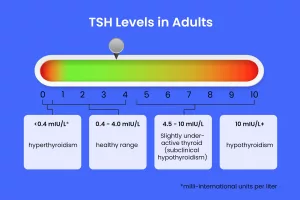
- Long‑term use: The NHANES analysis of over 5,000 U.S. adults found that regular cannabis users had lower TSH levels but no clinically meaningful thyroid dysfunction (Malhotra et al., 2017).
Study Comparison Table
| Study | Population | THC Dose | Duration | Thyroid Outcome |
|---|---|---|---|---|
| Healthline review (2025) | Mixed (healthy + hyperthyroid) | Variable | Acute | ↓ T3/T4 (short‑term) |
| Malhotra et al., 2017 | Cannabis‑dependent | Daily | 1 yr | No change in TSH/T3/T4 |
| NHANES 2007‑12 | General U.S. adults | Recent use | Past 30 days | ↓ TSH, no dysfunction |
Symptom‑Relief Perks
Anxiety & Mood Swings
THC can quiet the nervous system by calming the amygdala and boosting serotonin activity. Many people with hyperthyroidism describe feeling “on edge” all day—THC’s mellowing effect can feel like a gentle hand on a shaking steering wheel.
Sleep & Insomnia
If you’re lying awake while your heart races, a low dose of THC taken about 30 minutes before bed may help you drift off. Be aware, though: some folks experience paradoxical insomnia, so start tiny (2.5‑5 mg) and see how your body reacts.
Appetite & Weight Balance
Hyperthyroid patients often lose weight despite eating well. THC’s “the munchies” effect can give you a temporary boost in appetite—useful if you’re struggling to keep your calorie intake up.
Quick‑Tip Box: Gentle Dosing for Symptom Relief
- Start with 2.5 mg THC (a quarter of a standard gummy).
- Take it 30 minutes before bedtime for sleep, or mid‑day for anxiety.
- Wait at least 48 hours before adjusting the dose.
- Keep a simple journal: time, dose, symptoms, heart rate.
Risks & Side‑Effects You Shouldn’t Ignore
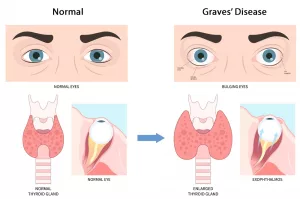
Thyroid‑Eye Disease (TED)
A 2025 ophthalmology study linked early THC use with a higher incidence of Graves’ ophthalmopathy—the eye‑bulging, pressure‑filled complication that can accompany hyperthyroidism (study). If you already have eye symptoms, proceed with extra caution.
Hormone Fluctuations & Tolerance
Regular, high‑dose THC can lead to tolerance, meaning the calming effect fades and you might increase the dose—potentially triggering rebound hormone spikes. A balanced approach (periodic breaks) helps keep things steady.
Psycho‑Active & Cardiovascular Concerns
THC can raise heart rate and blood pressure—already common in hyperthyroidism. If you have palpitations or a history of heart rhythm issues, discuss these risks with your doctor.
Side‑Effect Comparison Chart
| Factor | THC | CBD | Standard Treatment |
|---|---|---|---|
| Psycho‑active | Yes | No | No |
| Anxiety relief | ↑ (dose‑dependent) | ↑ | Variable |
| Impact on thyroid hormone | Slight ↓ (short‑term) | Minimal | Direct ↓ |
| Risk of eye disease | ↑ (early use) | None reported | None |
| FDA approval | None | Only Epidiolex (rare) | Yes |
CBD: The Non‑Psychoactive Cousin
Why Some Choose CBD Over THC
If the “high” sounds intimidating, CBD offers many of the same anti‑anxiety and anti‑inflammatory benefits without the intoxicating buzz. It interacts with the ECS in a more subtle way, which can be a gentler fit for folks who are pregnant, have a history of psychosis, or simply don’t want to feel “spaced out.”
What the Research Says
Evidence for CBD lowering thyroid hormones is still in its infancy. A 2022 review in Medical News Today noted that CBD may help with anxiety and sleep but didn’t find solid data on hormone modulation. In short, CBD can be a supportive ally but isn’t a direct thyroid‑treating agent.
When CBD Might Be a Better Fit
- You’re sensitive to THC’s psycho‑active effects.
- You have a history of eye pressure or glaucoma.
- You’re using other medications that could interact with THC.
Should You Try THC? A Practical Checklist
Step‑by‑Step Before You Light Up
- Confirm your diagnosis. Make sure recent labs (TSH, free T4) show hyperthyroidism.
- Talk to your endocrinologist. Ask about potential interactions with antithyroid drugs like methimazole.
- Check eye health. If you’ve been diagnosed with Graves’ ophthalmopathy, discuss the TED risk.
- Know the law. Verify that THC is legal in your state or country.
- Source safely. Purchase from a licensed dispensary that provides third‑party lab results for potency and contaminants.
Finding a Reliable Product
Look for these details on the packaging:
- Exact THC percentage (e.g., 5 %).
- Full cannabinoid profile (CBD, CBG, etc.).
- Certificates of analysis (COA) from an independent lab.
- Clear expiration date and storage instructions.
Real‑World Voices
Expert Insight (Suggested Quote)
“THC should never replace antithyroid medication. It can be an adjunct for symptom relief, but patients must be monitored for cardiovascular side effects and eye pressure,” says Dr. Maya Patel, MD, an endocrinologist at the University Thyroid Center.
Patient Story
Sarah, a 34‑year‑old teacher, shared: “When my thyroid storm hit, I could barely sleep. My doctor approved a tiny THC tincture (2 mg). After a week, I was finally able to catch some shut‑eye. The trade‑off was a slight buzzing feeling, so I trimmed the dose in half. My eye doctor kept a close eye on my vision, and nothing changed. I still take my prescription meds, but the THC helped me feel human again.”
Resources & Further Reading
- Healthline – Can THC Help with Hyperthyroidism?
- NHANES Cannabis & Thyroid Hormone Study (2017)
- 2025 Study on THC and Thyroid‑Eye Disease
- American Thyroid Association – Guidelines on Complementary Therapies (check the ATA website for the latest recommendation).
Conclusion
In a nutshell, THC can act like a soothing blanket for the anxiety, sleeplessness, and appetite changes that often accompany hyperthyroidism, but it’s not a cure. The biggest cautions are the limited research base, the potential to aggravate thyroid‑eye disease, and the psycho‑active side‑effects that might clash with an already racing heart.
The safest route is to bring any cannabis‑related plans to your endocrinologist’s table, start with the lowest possible dose, and keep a close eye on how you feel—and how your labs look. If you decide THC isn’t right for you, CBD or conventional medication remain solid, evidence‑backed options.
Have you tried THC or CBD for thyroid‑related symptoms? What was your experience? Drop a comment below or ask a question—you’re not alone on this journey.





















Leave a Reply
You must be logged in to post a comment.