If you’ve just heard “underactive thyroid” from your doctor, you’re probably wondering whether you really need to start a pill every morning. The short answer? Most people with hypothyroidism do benefit from a thyroid‑hormone replacement medication, and the right dose can turn a foggy, sluggish life into something bright and energetic again. In this post we’ll walk through exactly what that medication does, how it’s prescribed, what you can expect, and how to stay safe—all written in a casual, friend‑to‑friend tone.
Why Medication Matters
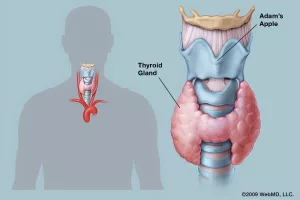
Think of your thyroid as the body’s thermostat. When it’s working, it keeps your metabolism humming at the perfect temperature. When it’s underactive, the thermostat is stuck on “cold,” and you feel the chill in every part of your day—fatigue, weight gain, brain fog, and that dreaded “I’m always cold” feeling. Medication restores the missing hormone so your internal thermostat can finally do its job.
How Replacement Works
Most hypothyroidism medication is levothyroxine, a synthetic form of the hormone thyroxine (T4). According to WebMD, levothyroxine “provides a source of thyroid hormone in people who may not make enough on their own.” Once you swallow a tablet, your body converts the T4 into the more active triiodothyronine (T3) where it’s needed, essentially filling the gap left by an underactive gland.
Do I Need T3 Too?
Only a small subset of patients benefit from a direct T3 supplement (liothyronine) or a combination of T4 + T3. As NYU Langone notes, “a small number of patients may need a combination of levothyroxine and liothyronine to feel their best.” Most doctors start you on levothyroxine alone and only consider adding T3 if you continue to feel sluggish despite normal lab numbers.
Comparison Table
| Form | Typical Dose Range | Half‑Life | Common Use |
|---|---|---|---|
| Levothyroxine (T4) | 25‑200 µg daily | ≈ 7 days | First‑line for most hypothyroidism |
| Liothyronine (T3) | 5‑25 µg daily | ≈ 1 day | Adjunct for select patients |
| Combination (T4 + T3) | Varies; often 75‑125 µg T4 + 5‑10 µg T3 | Mixed | Patients not fully improved on T4 alone |
The Core Drug
Names & Forms
Levothyroxine ships under many brand names—Synthroid, Levoxyl, Tirosint, Ermeza, and a handful of generics. It’s available as tablets, capsules, and even a liquid solution for those who struggle with swallowing pills. The variety lets you pick the form that fits your lifestyle best.
Typical Dosage & Adjustments
Doctors usually start low, especially if you have heart disease or are older, then increase the dose every 4–6 weeks based on bloodwork. A common starting point is 25‑50 µg per day, with gradual titration up to 125‑150 µg for many adults. If you’re pregnant, your dose may need a 20‑30 % bump because estrogen raises thyroid‑binding globulin—a fact highlighted in the American Thyroid Association guidelines.
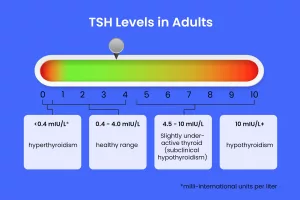
Monitoring Labs
The primary lab you’ll hear about is TSH (thyroid‑stimulating hormone). After a dose change, doctors wait about 4‑6 weeks for TSH to settle before checking again. Your target is usually 0.5‑4.0 mIU/L, but individual goals may differ. Free T4 is also measured to ensure you’re not over‑replacing.
Sample Dosing Schedule
| Week | Starting Dose | Adjustment | Rationale |
|---|---|---|---|
| 0‑4 | 25 µg | None | Assess tolerance, especially heart rate |
| 5‑8 | 50 µg | Increase if TSH > 4 | Gradual rise avoids cardiac stress |
| 9‑12 | 75 µg | Adjust up/down | Fine‑tune to target TSH |
| 13‑16 | 100 µg | Modify as needed | Most adults land here |
Benefits You’ll Feel
Symptom Relief Timeline
Most people start noticing a lift in energy within a week, and mood improvements usually follow in 2‑3 weeks. Full normalization of cholesterol and weight can take a few months, but the early “I can finally get out of bed” sensation is a real win.
Real‑World Stories
Let me share a quick anecdote. My friend Maya, 42, was diagnosed after a routine blood test that showed a high TSH. She began on 75 µg of levothyroxine, and by the end of the second week she could finally finish her morning jog without feeling winded. Two months later, her doctor reduced her dose slightly after a tiny TSH dip, and she’s now on a maintenance dose that lets her feel “back to herself.” Stories like Maya’s remind us that the right dose really can change a life.
Risks & Side Effects
Over‑ vs Under‑Replacement
Taking too much can mimic hyperthyroidism—fast heartbeat, nervousness, and even bone loss over time. Conversely, an under‑dose leaves you with lingering hypothyroid symptoms. WebMD flags “arrhythmias” as a serious concern when levothyroxine is over‑administered, especially in older adults.
When to Call Doctor
If you experience chest pain, rapid or irregular heartbeat, severe anxiety, or sudden weight loss, contact your provider ASAP. These could signal an overdose.
Red‑Flag Checklist
- Chest discomfort or palpitations
- Sudden tremor or shakiness
- Unexplained weight loss > 5 lb in a week
- Severe headache or vision changes
- Persistent diarrhea or vomiting
Special Populations
Pregnancy & Children
During pregnancy your thyroid needs increase, so you’ll likely need a higher dose. Children, especially those who had thyroid surgery, often stay on levothyroxine for life, with doses calculated by weight (µg/kg). Monitoring is tighter because growth and brain development depend on stable thyroid levels.
Elderly & Heart Issues
Older adults are more prone to heart‑related side effects, so doctors start as low as 12.5 µg and increase slowly. If you have a history of atrial fibrillation, your doctor will be extra cautious.
Dosage Tweaks Table
| Group | Starting Dose | Adjustment Speed | Key Monitoring |
|---|---|---|---|
| Pregnant | Increase 20‑30 % | Every 4 weeks | TSH, free T4 |
| Children | 1‑2 µg/kg | Every 6‑8 weeks | Growth, TSH |
| Elderly | 12.5 µg | Slow titration | Heart rate, ECG |
| Heart disease | ≤25 µg | Very gradual | BP, rhythm |
Tips for Taking It Right
Absorption Hacks
Levothyroxine likes an empty stomach. Take it with a full glass of water, 30‑60 minutes before breakfast. Avoid calcium, iron, coffee, or high‑fiber foods within four hours, as they can bind the pill and reduce absorption.
Do‑and‑Don’t List
- Do use the same brand every day (switching can change bioavailability).
- Do store tablets at room temperature, away from light.
- Don’t crush or chew the tablet—unless you’re on a liquid form prescribed for that reason.
- Don’t skip a dose; if you miss one, take it as soon as you remember unless it’s close to the next dose.
Action Plan for You
Step‑by‑Step Guide
- Get confirmed labs. A TSH and free T4 test will tell you where you stand.
- Start low, go slow. Follow your doctor’s initial dose and give it 4‑6 weeks before the next blood draw.
- Track symptoms. Keep a simple journal: energy level, temperature tolerance, mood, and any side effects.
- Check labs again. Adjust based on the newest TSH result.
- Know the red flags. If any checklist items appear, call your clinician right away.
- Stay consistent. Take the pill at the same time each day; consistency equals stability.
Remember, you’re not alone in this journey. Thousands of people navigate hypothyroidism medication every day, and the community of patients, doctors, and pharmacists is there to guide you. If you ever feel stuck, reach out to your endocrine specialist, ask about a dose review, or simply share your experience in an online support group. Your voice matters, and your health is worth the effort.
Bottom line: Hypothyroidism medication—most often levothyroxine—offers a safe, effective way to replace missing thyroid hormone, lift the fog, and protect long‑term health. By understanding how it works, monitoring carefully, and following a few simple tricks, you can turn a diagnosis into a roadmap for feeling your best.
What’s your experience with thyroid medication? Have you discovered any personal tricks that help you stay on track? Drop a comment below or share your story with a friend who might need a little encouragement. We’re all in this together!




















Leave a Reply
You must be logged in to post a comment.