A tracheostomy speaking valve redirects air away from your tracheostomy so you can speak with greater ease. Both you and your caregivers will need instruction on how to clean and look after the valve safely.
These speaking valves reroute airflow through your vocal cords, enabling you to produce voice.
A tracheostomy alters pressure dynamics in your airway, changing how air flows across the vocal cords and making clear speech challenging. Speaking valves for tracheostomies address this issue and can offer additional advantages, such as enhancing swallowing.

Continue reading to find out more about tracheostomy speaking valves, the benefits they provide, and how to maintain them.
What is a tracheostomy speaking valve?
A tracheostomy speaking valve is a one-way device that prevents air from escaping through the tracheostomy when you exhale.
After a tracheostomy is placed, much of your exhaled air leaves via the tracheostomy tube rather than moving up through the vocal cords. This change in airflow makes producing speech difficult.
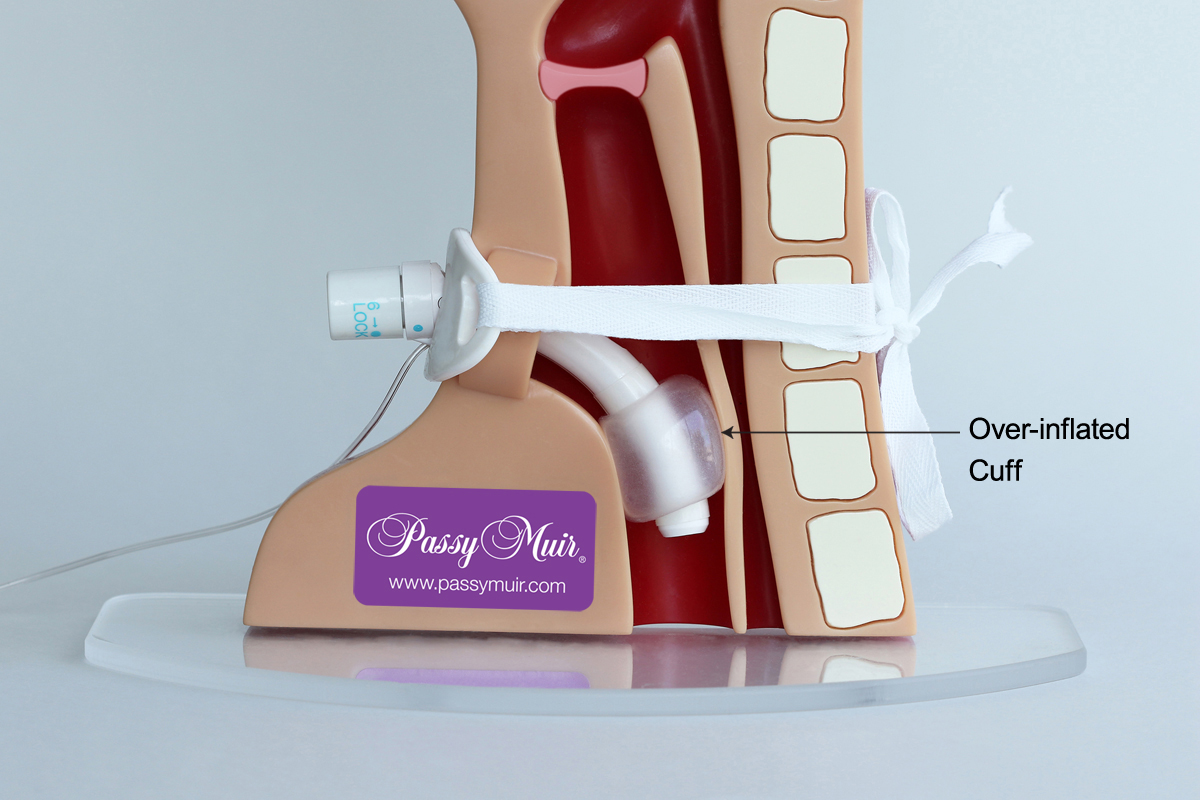
The most commonly used speaking valve is the Passy-Muir swallowing and speaking valve (PMV), named for its creator David Muir.
Speaking with a tracheostomy tube
Tracheostomies may be temporary or permanent. Regardless of duration, loss of speech can have significant negative effects. Inability to converse with family can cause depression, social withdrawal, and reduced morale.
Not being able to communicate with healthcare staff can also negatively affect recovery and participation in rehabilitation.
A speaking valve can channel air back through your vocal cords, offering benefits such as:
- letting you speak with your natural voice
- increasing vocal loudness
- enhancing the rhythm and clarity of speech

How does a speaking valve help?
Speaking valves can be essential for helping people with tracheostomies regain verbal communication. Beyond improving speech, they may provide additional benefits, including:
- better swallowing ability
- reduced aspiration (when food or liquid enters the lungs)
- lowering your pneumonia risk — which is about 11 times more likely in people who aspirate
- enhancing taste and olfactory sensations
- assisting with secretion control, potentially reducing suctioning needs
- decreasing dependence on mechanical ventilation by improving lung volumes, enhancing diaphragm movement, and supporting alveolar function
Who is a good candidate for a speaking valve?
Many individuals with tracheostomies are suitable candidates for speaking valves.
According to Passy-Muir, eligible users include people who are:
- conscious and responsive
- of any age
- using a ventilator
- not using a ventilator
People who aren’t candidates for a speaking valve
Individuals who aren’t suitable for the PMV include those with:
- reduced or absent consciousness
- a tracheostomy tube cuff that is inflated
- a cuffed tracheostomy tube filled with foam
- severe airway obstruction
- thick or copious secretions in the upper airway
- markedly decreased lung compliance
- endotracheal tubes in place
Learning to use a tracheostomy speaking valve
Adapting to a speaking valve may take time. Your physician may refer you to a speech-language pathologist to guide you. It’s crucial that you, family members, and caregivers understand correct use and care of the valve.
You may collaborate with speech therapists, occupational therapists, and other clinicians to learn to use the device.
A speech-language pathologist can help you:
- gradually increase the duration you wear the speaking valve
- enhance voice quality
- improve coordination between breathing and speaking
Some organizations, such as Tracheostomy Education, offer tools to help children practice using their speaking valves.
If you’re exploring related accessories or care components, you might also find helpful information about what is a tracheostomy collar that can complement trach care.
Maintaining your trach and speaking valve
It’s often advised to have two speaking valves so you can swap them for cleaning and drying.
The Passy-Muir guidelines state each valve should last at least two months with proper upkeep.
To clean your speaking valve:
- Gently swish the valve in warm, soapy water (not hot).
- Rinse the valve thoroughly under warm running water.
- Let the valve air dry completely before placing it in its storage case.
Avoid using:
- hot water
- bleach
- vinegar
- alcohol
- brushes
- peroxides
- cotton swabs
Potential risks
When used correctly, speaking valves have a generally favorable safety profile. A 2020 study reported no adverse effects with use up to 17 hours in a day.
Although uncommon, risks can stem from improper use. For example, ensure the tracheostomy tube cuff is deflated before using a PMV. Also, do not confuse the PMV with a heat and moisture exchanger, which appears similar but lacks the one-way valve mechanism.
Frequently asked questions about the tracheostomy speaking valve
Below are common questions people have about tracheostomy speaking valves.
Can anyone with a tracheostomy use a speaking valve?
Many people with tracheostomies can use speaking valves, but not everyone. Those in a coma or with severe airway obstruction are examples of people who typically aren’t suitable candidates.
How often should the speaking valve be replaced?
Each Passy-Muir valve is intended to last at least two months. Replace the valve sooner if it becomes sticky, noisy, or begins to vibrate.
How do you clean a tracheostomy speaking valve?
Clean the valve with warm, soapy water, rinse well, and allow it to air dry. Avoid brushes, cotton swabs, and any cleaners that could leave residue.
Takeaway
A speaking valve is a one-way device that closes your tracheostomy when you exhale, directing air upward through your vocal cords and enabling speech.
Speaking valves can also enhance swallowing and may improve smell and taste. Many individuals with tracheostomies who are alert and responsive are eligible to use a speaking valve.























Leave a Reply
You must be logged in to post a comment.