Ever caught a glimpse of yourself in the mirror and thought, “Why does my face look so puffy today?” You might be surprised to learn that an over‑active thyroid can paint its own portrait on your skin, eyes, and even the hair on your head. In the next few minutes we’ll walk through the most common hyperthyroidism facial symptoms, why they happen, and how getting the right treatment can bring your reflection back to normal. Grab a coffee, settle in, and let’s figure this out together.
Why Face Changes
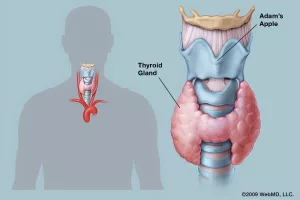
First things first – why does the thyroid, a tiny butterfly‑shaped gland tucked under your chin, have such a big say in how your face looks? The answer lies in two main mechanisms that most medical sources agree on.
Metabolism on Overdrive
When the thyroid pumps out too much hormone, your body’s metabolism revs up like a sports car on a highway. Blood vessels dilate, blood flow increases, and extra fluid can collect in the soft tissues around the eyes, nose, and cheeks. This is why many people describe the swelling as “puffy” or “full‑filled.” Healthline explains that this fluid retention is especially common around the eyes, giving a “puffy‑eye” look.
Autoimmune Inflammation
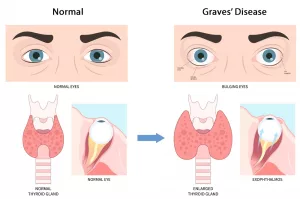
Most cases of hyperthyroidism stem from Graves’ disease, an autoimmune condition where the immune system mistakenly attacks thyroid cells – and sometimes the tissues behind the eyes. This inflammation can push the eyeballs forward (exophthalmos) and irritate the delicate skin on the face. The American Academy of Ophthalmology calls this the classic “thyroid stare.”
Quick Metabolism vs. Inflammation Chart
| Trigger | Facial Effect | Typical Timeline |
|---|---|---|
| Increased metabolism | Swelling, warm skin, flushing | Days to weeks |
| Autoimmune eye inflammation | Bulging eyes, dry/redness | Weeks to months |
Core Facial Symptoms
Now that we know the “why,” let’s talk about the “what.” Below is the checklist most doctors use when they suspect hyperthyroidism based on a patient’s look.
Facial Puffiness & Edema
Imagine waking up with a slightly “ballooned” appearance around your cheeks and under‑eye area. It’s not just extra makeup – it’s genuine fluid buildup. If it lingers beyond a couple of weeks, it’s worth mentioning to your physician.
Exophthalmos (Bulging Eyes)
Ever seen a friend whose eyes seem a little wider than usual, as if they’re constantly “staring”? This is called exophthalmos or “thyroid eye disease.” It can make it hard to close the lids completely, leading to dryness and a gritty feeling. According to the American Academy of Ophthalmology, about 20% of people with Graves’ disease develop this eye change.
Skin Changes
- Warm, moist, thin skin: The skin often feels hotter than usual, almost as if you just stepped out of a shower.
- Redness or flushing: Some describe a “sun‑kissed” hue that appears without any sun exposure.
- Rashes & hives: Occasionally, tiny itchy welts appear on the face and neck, known as a hyperthyroidism rash.
- Hyperpigmentation: Darker patches can develop, especially on the neck and the back of the hands.
Hair Loss & Thinning
Notice your eyebrows looking a little sparser or your scalp shedding more than usual? Thyroid hormones accelerate the hair‑growth cycle, which can send more hairs into the “resting” phase, resulting in noticeable thinning on the scalp, eyebrows, and even eyelashes.
Neck Swelling (Goiter)
A visible lump at the base of the neck is a classic sign. While a goiter itself isn’t a facial symptom, its presence often goes hand‑in‑hand with the facial changes we’re discussing. If you can feel a “balloon” sensation under your chin, it’s time for a professional check.
Symptom Summary Table
| Symptom | Description | When to Seek Care |
|---|---|---|
| Facial puffiness | Swelling around eyes, cheeks, nose | Persistent > 2 weeks |
| Bulging eyes | Protruding eyeballs, stare‑like appearance | Sudden change or vision issues |
| Skin warmth/redness | Hot, moist skin; flushing | Accompanied by rash or itching |
| Hair thinning | Sparse eyebrows, lashes, scalp hair loss | Rapid loss over weeks |
| Neck swelling | Visible lump or fullness at throat | Any size with discomfort |
Spotting the Signs Early
Think of it like a morning routine for your face: a quick mirror check, noting any new puffiness, dryness, or changes in hair density. Write down when you first saw it, how long it lasts, and any triggers (like stress or a new medication). This “symptom log” becomes a powerful tool when you talk to your doctor.
Related Thyroid Changes
Facial signs rarely act alone. They often sit alongside other systemic clues that, together, paint a clear picture of hyperthyroidism.
Thyroid Face vs. Thyroid Eye Disease
“Thyroid face” is a lay term describing the combination of puffiness, skin changes, and a noticeable goiter. In contrast, “thyroid eye disease” or Graves’ eye disease zeroes in on the orbital inflammation that causes bulging eyes. Both stem from the same hormonal imbalance, but they may require slightly different specialists – an endocrinologist for the systemic picture and an ophthalmologist for the eye involvement.
Rashes vs. Other Skin Conditions
Many people mistake a hyperthyroidism rash for an allergic reaction. The key difference? Thyroid‑related rashes often appear on the face, neck, and sometimes the torso, and they tend to improve once hormone levels are controlled.
Medication Side‑Effects
Some antithyroid medicines (like propylthiouracil) can cause skin redness or mild swelling as a side‑effect. If you start a new pill and notice a rash, let your doctor know – it might be the medication, not the thyroid itself.
Getting Proper Diagnosis
Seeing an odd change in your reflection can be unsettling, but the path to clarity is straightforward.
What the Doctor Looks For
- Physical exam: Palpation of the thyroid gland, checking for eye bulging, skin temperature, and measuring any facial edema.
- Blood tests: TSH (thyroid‑stimulating hormone), free T4, free T3, and sometimes thyroid‑stimulating immunoglobulins (TSI) to confirm Graves’ disease.
- Imaging: Ultrasound of the thyroid or a radioactive iodine uptake scan if the cause isn’t obvious.
When to See an Endocrinologist or Ophthalmologist
If you notice any eye‑related changes – especially double vision, persistent dryness, or a visible “stare” – schedule an appointment with an ophthalmologist. For the rest of the symptoms, an endocrinologist can guide you through hormone testing and treatment options.
Sample Patient Questionnaire (downloadable)
Feel free to copy these prompts into a note on your phone:
- When did you first notice facial swelling?
- Any recent weight loss, rapid heartbeat, or heat intolerance?
- Do you feel anxiety or have trouble sleeping?
- Any family history of thyroid disease?
Treatment Options
Good news: most hyperthyroidism facial symptoms improve once the hormone excess is tamed. The right treatment depends on the cause, severity, and your personal preferences.
Antithyroid Medications
Drugs like methimazole or propylthiouracil block the thyroid’s ability to produce excess hormone. Many patients notice a reduction in facial puffiness within 2–4 weeks of consistent use.
Radioactive Iodine Therapy
This single‑dose treatment shrinks the thyroid by destroying overactive cells. It’s very effective, though some people experience a temporary flare‑up of eye symptoms before they settle down. Healthline notes that swelling often eases within a few months after the procedure.
Surgical Options
When medication or iodine isn’t enough, a surgeon can remove part (lobectomy) or all (total thyroidectomy) of the gland. Post‑surgery, you’ll need lifelong thyroid‑hormone replacement, but most facial changes resolve permanently.
Targeted Eye‑Disease Therapies
- Corticosteroids: Reduce orbital inflammation quickly.
- Orbital radiation: Helps when steroids alone aren’t sufficient.
- Decompression surgery: In severe cases, extra bone is removed to give the eyes more space.
Supportive Skin‑Care & Lifestyle Tweaks
While medication does the heavy lifting, gentle skin‑care can soothe discomfort:
- Use fragrance‑free, hydrating cleansers.
- Apply a moisturizer with ceramides after washing.
- Stay hydrated – water helps reduce fluid retention.
- Consider foods rich in selenium (Brazil nuts) and vitamin D, both linked to healthier thyroid function.
Before & After Treatment Comparison
| Treatment | Typical Time to See Facial Improvement | Potential Eye‑Specific Action |
|---|---|---|
| Antithyroid meds | 2–4 weeks | Often none needed |
| Radioactive iodine | 1–3 months | May need steroids for eye flare |
| Surgery | Immediate hormone control | Eye disease may still need separate care |
Real‑World Stories
Statistics are useful, but personal stories bring the facts home. Below are two anonymized experiences that illustrate how facial symptoms can change – and improve – with proper care.
Case A: The “Puffy‑Cheek” Surprise
Emily, 32, first noticed that her cheekbones looked fuller after a stressful work period. She thought it was just stress‑related water retention, but the puffiness persisted for a month. A quick symptom log helped her doctor order thyroid labs, which revealed low TSH and high free T4. After starting methimazole, Emily’s cheek swelling faded within three weeks, and her energy levels rose back to normal. “I felt like I finally recognized myself in the mirror again,” she says.
Case B: The “Staring” Dilemma
Mark, 58, was diagnosed with Graves’ disease two years ago. He managed his hormone levels with radioactive iodine, but his eyes continued to protrude, giving him a permanent “stare.” An ophthalmologist prescribed a short course of oral steroids, followed by orbital radiation. Six months later, the bulge reduced noticeably, and Mark no longer needed to squint to keep his eyes closed at night. “It wasn’t just about looking better – it was about not feeling self‑conscious in meetings,” he explains.
Talk to Your Doctor
Feeling equipped with knowledge is empowering, but the next step is a conversation with a healthcare professional. Here are a few tips to make that chat as productive as possible:
- Bring your symptom log: Dates, severity, triggers – the more detail, the better.
- Ask specific questions: “Which blood tests will confirm whether my facial changes are thyroid‑related?” or “If my eyes are affected, should I see an ophthalmologist right away?”
- Discuss treatment side‑effects: “Will the medication I start cause any skin irritation?”
- Request a referral if needed: Don’t hesitate to ask for an eye specialist if you notice any vision changes.
Quick Resources
For a deeper dive, these trusted sources offer up‑to‑date, evidence‑based information (links open in a new tab):
- Healthline’s overview of hyperthyroidism facial symptoms
- American Academy of Ophthalmology’s guide to thyroid eye disease
- Frontiers study on metabolic mechanisms behind facial swelling
Conclusion
Facial changes can be one of the first clues that your thyroid is running a little too fast. From puffiness and bulging eyes to skin warmth, hair thinning, and a noticeable goiter, these hyperthyroidism facial symptoms are more than skin‑deep – they signal a systemic imbalance that deserves attention. The encouraging news is that, with the right diagnosis and treatment, most people see a marked improvement within weeks to months.
If any of the signs above sound familiar, consider starting a symptom journal and scheduling a visit with your doctor. You don’t have to live with a face that feels “off.” Together with a trusted healthcare team, you can bring your reflection back into alignment and reclaim the confidence you deserve.
What’s your experience with thyroid‑related facial changes? Have you found a particular skin‑care routine helpful? Share your thoughts in the comments below – we’re all in this together.





















Leave a Reply
You must be logged in to post a comment.