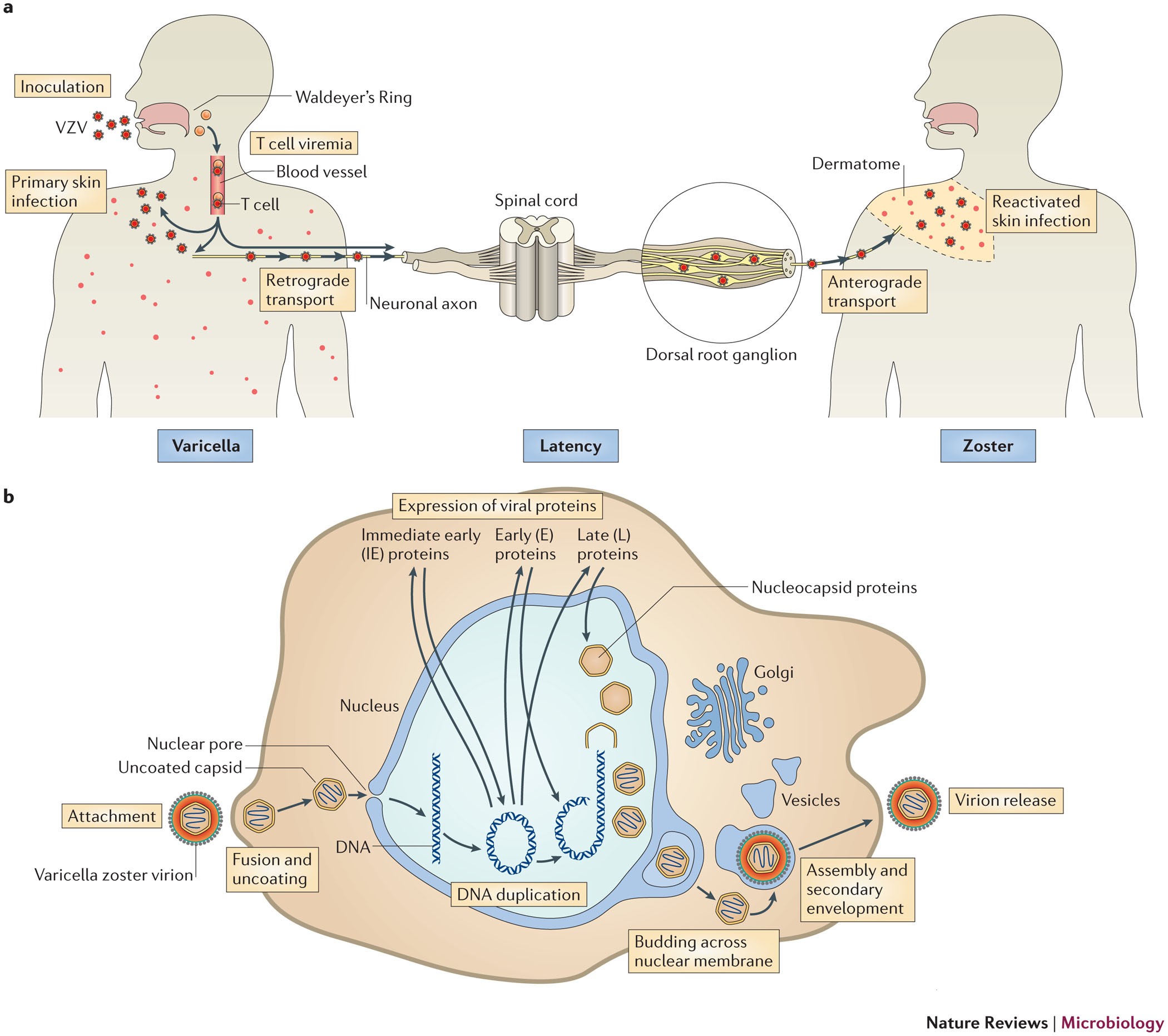
When the varicella-zoster virus becomes active again, it moves along a defined nerve route. This explains why a shingles rash often appears in one or more regions supplied by that nerve. That specific skin area along the nerve route is called a dermatome.
Shingles, or herpes zoster, occurs from reactivation of the varicella-zoster virus — the same virus responsible for chickenpox.
After an initial chickenpox infection, the virus typically remains inactive for years within nerve cells. If it reactivates, it travels down particular nerve pathways until it reaches the skin. At that point, a blistering rash develops that leaves a linear pattern and produces pain and itching.
The rash can develop on any part of the body but most commonly appears on one side of the trunk or torso. Where the shingles rash shows up depends on which nerve the virus spreads from. Typically, the rash is confined to one or two dermatomes.
If you’ve never had chickenpox, direct contact with someone’s active shingles rash may give you chickenpox. If you already had chickenpox, exposure to the reactivated virus can instead trigger shingles.
The connection between shingles and nerve routes
The first time you encounter the varicella-zoster virus, you develop chickenpox. After recovery, the virus persists in an inactive form. It commonly remains dormant in your cranial nerves and spinal ganglia. Spinal ganglia are clusters of nerve cells that link your spinal cord to the nerves of your body and limbs.
If the varicella-zoster virus reawakens years later, it spreads along sensory nerve fibers from the spinal cord toward regions of the skin. This process manifests as shingles.
Nerves transmit sensory signals. They carry messages of pain, itch, or pressure from the skin to the spinal cord and brain.
When the virus travels along a nerve and reaches the skin, it commonly produces a painful, itchy rash. Besides the visible blistering rash, the virus can create sensations along that nerve route, such as burning pain, tingling, and itching. These symptoms can also occur when shingles present without an obvious rash.
Shingles can last up to five weeks.
You can learn more about early signs of shingles here.

What are dermatomes?
A dermatome is a skin region where sensation is provided by a single spinal nerve.
You have 31 spinal nerves on each side of your body that relay information between your body and spinal cord. Each of these nerves corresponds to a dermatome, except for the C1 spinal nerve in the neck.
For instance, the right C5 spinal nerve conveys sensory input from the right collarbone and upper shoulder to the spinal cord and brain. The skin in that area constitutes one dermatome.
Shingles rashes typically form along one or two dermatomes on a single side of the body. Their placement reflects which nerve the virus propagated from. The rash generally does not cross the body’s midline because each spinal nerve supplies sensation only to either the left or right side.
How shingles impact nerve pathways
Shingles provoke inflammation and temporary dysfunction in affected nerves, producing symptoms such as burning pain, itching, numbness, and a rash. As the herpes zoster virus progresses along sensory nerves, it can cause more extensive damage and inflammation, sometimes persisting after the rash has cleared. Many complications of shingles stem from this nerve injury.
You can read more about shingles pain here.
Postherpetic neuralgia
The most frequent long-term complication of shingles is postherpetic neuralgia — persistent pain or itching that continues for weeks or months after the rash resolves. This condition results from nerve damage.
Most people recover from postherpetic neuralgia within a year, though in some cases the pain can be permanent.
Motor nerve injury
The varicella-zoster virus can also target motor nerves that control muscle movement. It is estimated that about 0.5–5% of people with shingles develop segmental zoster paresis, which causes weakness in muscles near the shingles rash.
Cranial nerve involvement
Occasionally, the herpes zoster virus affects one of the major cranial nerves in the head. Fewer than 1% of shingles cases involve cranial nerve VII (the facial nerve), resulting in facial shingles. One potential complication is Ramsay Hunt syndrome.
This syndrome may cause symptoms such as:
- paralysis of one side of the face
- ear pain
- blisters in or around the ear
- altered taste in the front two-thirds of the tongue
- dry eyes
- hearing loss
- vertigo
- tinnitus
How is nerve injury treated?
Medications are the primary approach for treating long-term pain and weakness caused by nerve injury. Shingles treatment aims to lessen symptom severity and duration and reduce the risk of complications. When complications like nerve damage occur, clinicians may recommend the following:
Anticonvulsants
Anticonvulsant medications, such as gabapentin and pregabalin, are FDA-approved for treating postherpetic neuralgia. These agents act on calcium channels and modulate neurotransmitter release to ease pain.
Antidepressants
Various antidepressants, given at low doses, can help manage chronic pain. Tricyclic antidepressants are a commonly used class for this purpose; they work by inhibiting the reuptake of serotonin and norepinephrine.
Topical local anesthetics
Two topical options are frequently used to manage nerve pain. Lidocaine is FDA-approved specifically for postherpetic neuralgia.
Capsaicin cream is available over the counter and can be modestly effective, though many individuals report a burning sensation when applying it.
A healthcare provider may also prescribe additional pain-relieving medications.
Optum Now is operated by RVO Health. By clicking on this link, we may receive a commission. Learn more.
Takeaway
The chickenpox virus can lie dormant in nerves for many years and later reactivate as shingles. When reawakened, the virus reaches the skin by traveling along specific nerve pathways. A shingles rash appears in the skin area governed by that particular nerve.
Because the shingles virus follows nerves that convey pain, pressure, and temperature signals to the brain, the condition is often painful and uncomfortable. The rash typically traces a line, usually along one or two nerve pathways on a single side of the face or body.


















Leave a Reply
You must be logged in to post a comment.