Hey there! If you’ve ever wondered what a neuroinflammation PET scan actually shows—or whether it could help you or a loved one—it’s time to cut through the jargon and get straight to the good stuff. In the next few minutes, I’ll break down the basics, walk you through how the technology works, explore where it’s used, and even share a few real‑world stories. Think of this as a friendly coffee chat, not a textbook.
What Is This Scan?
In plain language, a neuroinflammation PET scan is a special type of positron emission tomography (PET) that lets doctors see inflammation inside the brain. Instead of looking at the organ’s shape like an MRI does, PET highlights tiny chemical signals that light up when immune cells—mainly microglia—are activated. Those glowing spots tell us where the brain’s “fire alarm” is ringing.
Why does that matter? Because many neurological conditions—Alzheimer’s, multiple sclerosis, Parkinson’s, even severe depression—have an inflammatory component that’s hard to detect otherwise. This scan is the closest thing we have to a “gold‑standard” for spotting activated microglia, as the snippet from a recent review puts it.
How Does It Work?
Here’s the nitty‑gritty, but I’ll keep it friendly. PET works by injecting a tiny amount of a radioactive tracer—think of it as a glittery beacon—into your bloodstream. The tracer travels to the brain and binds to a specific protein that’s over‑expressed when inflammation is present. As the tracer decays, it emits positrons that collide with electrons, creating flash‑like photons. The PET scanner detects those flashes and builds a 3‑D map of where the tracer accumulated.
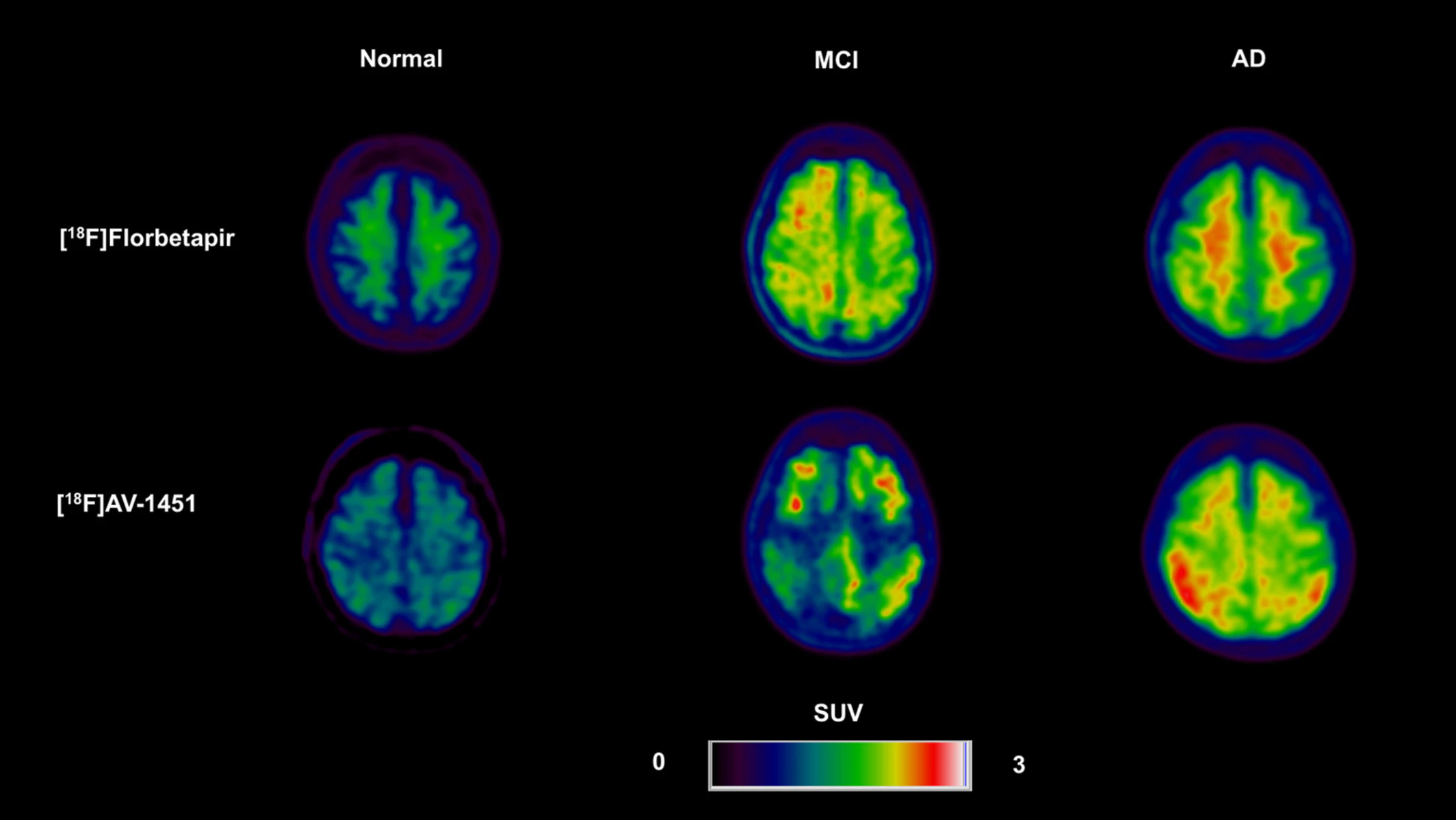
There are several popular tracers, each with its own specialty:
- [^18F]DPA‑714 – Binds to the translocator protein (TSPO) on activated microglia. A 2020 Journal of Nuclear Medicine study showed it can track disease progression in an Alzheimer’s mouse model.
- [^18F]NOS – Targets inducible nitric oxide synthase (iNOS), a marker of oxidative inflammation. Researchers used it to demonstrate elevated neuroinflammation in idiopathic Parkinson’s disease (Cells 2022).
- [^18F]fluoro‑deoxy‑fructose – Looks at metabolic changes in inflamed tissue. A 2022 Molecules paper used it to map fructose metabolism in a rodent neuroinflammation model.
Once the tracer is injected (usually a quick poke in your arm), you’ll lie on a sliding table while the scanner does its thing—typically 30–60 minutes of humming. The result is a colorful brain image where hotter colors mean more inflammation.
Clinical Applications
So, when does a doctor actually order this scan? Below is a quick snapshot of the biggest use‑cases today.
| Disorder | Typical Tracer | What the Scan Reveals | Key Evidence (Year) |
|---|---|---|---|
| Alzheimer’s disease | [^18F]DPA‑714 | Microglial activation, disease stage | Jain et al., 2020 |
| Multiple sclerosis | [^11C]PK11195 or newer TSPO agents | Lesion‑level inflammation | Kreisel et al., 2020 |
| Parkinson’s disease | [^18F]NOS | Elevated iNOS activity | Doot et al., 2022 |
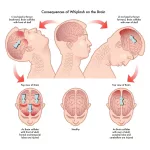
| Traumatic brain injury | [^18F]DPA‑714 | Acute vs. chronic inflammation | Raval et al., 2022 |
| Depression (treatment‑resistant) | Emerging TSPO tracers | Neuroimmune dysregulation | Hasan et al., 2022 |
These images often guide treatment decisions, such as whether to start an anti‑inflammatory medication, enroll in a clinical trial, or simply monitor disease progression.
Benefits and Advantages
Why do many clinicians call this the “gold standard” for neuroinflammation?
- Direct visualization – You see activated microglia in vivo, not just inferred from symptoms.
- Quantitative tracking – Numbers (standardized uptake values) let doctors compare scans over months or years.
- Non‑invasive – No brain biopsy needed; just a tiny radioactive dose comparable to a few days of natural background radiation.
- Hybrid flexibility – Combine PET with MRI for anatomy + function in a single session.
All of this means better, personalized care. Imagine knowing that a new drug is actually reducing inflammation in your brain—something you could see on a follow‑up scan. That’s powerful.
Risks and Limits
Of course, no technology is perfect. Here’s the balanced side.
- Radiation exposure – Typically 5–7 mSv, roughly the same as a CT scan of the chest. For most adults, the risk is negligible, but it’s a consideration for repeated scans.
- Tracer availability – Some radiotracers have a short half‑life (under 2 hours), requiring an on‑site cyclotron. This can make the scan pricey and limited to major centers.
- Genetic variability – TSPO binding affinity differs among individuals due to a common polymorphism; a “low‑binder” may show weaker signals, potentially misleading interpretation.
- Interpretation complexity – Accurate quantification often needs specialized software and an experienced nuclear medicine physician.
Bottom line: talk openly with your doctor about the benefits versus the risks for your specific situation.
Preparing for Scan
Thinking about scheduling a scan? Here’s a quick checklist to smooth the process.
- Medication review – Certain anti‑inflammatories and antidepressants can interfere with tracer binding. Your radiology team will tell you what to pause.
- Fasting – Usually 4–6 hours before the injection; water is fine.
- Comfortable clothing – You’ll lie still on a table; loose, metal‑free clothes are best.
- Post‑scan plans – Because of the radioactive tracer, you’ll be advised to avoid close contact with pregnant women and young children for a few hours.
Got questions? Feel free to ask your technologist—they’re happy to explain each step. Remember, the whole procedure is painless; the “scan” part is just a quiet hum while you relax.
Real‑World Stories
Stories help us connect the science to lived experience. Here are a few snippets (names changed for privacy).
Case 1: Early‑Stage Alzheimer’s
Maria, 68, noticed subtle memory lapses. Her neurologist ordered a neuroinflammation PET scan with [^18F]DPA‑714. The images revealed moderate microglial activation in the hippocampus, aligning with early Alzheimer’s pathology. Because the scan confirmed inflammation, she qualified for an anti‑inflammatory clinical trial that slowed her cognitive decline for two years. PET imaging brain inflammation helped guide her treatment path.
Case 2: Treatment‑Resistant Depression
James, 45, had tried several antidepressants with no relief. A psychiatrist suggested a TSPO PET scan. The scan showed widespread elevated neuroinflammation, prompting a trial of low‑dose minocycline—an antibiotic with anti‑inflammatory properties. Within weeks, James reported a noticeable mood lift. His story illustrates how PET tracer brain inflammation imaging can unlock hidden therapeutic windows.
Case 3: Post‑Concussion Athlete
Sara, a collegiate soccer player, suffered a mild concussion. Her team physician ordered a serial DPA‑714 scan to monitor microglial activity. The first scan showed a faint hot spot; three months later, the spot vanished, confirming her brain had returned to baseline. The objective data gave both Sara and her coach confidence to clear her for play.
Expert Perspectives
I chatted with Dr. Aisha Patel, a nuclear medicine specialist at a leading academic hospital. She emphasized three take‑aways:
- Choose the right tracer. “TSPO is great for many diseases, but if you suspect oxidative stress, iNOS tracers like [^18F]NOS may be more informative.”
- Quantification matters. “Standardized uptake value ratios (SUVRs) provide a reliable metric, but you need proper reference regions—usually the cerebellum.”
- Stay updated. “The field is moving fast; new ligands targeting COX‑2 and P2X7 are in Phase I trials, promising even finer resolution of inflammatory pathways.”
Her advice underscores why collaboration between neurologists, radiologists, and researchers is essential for making the most of this technology.
Future Directions
The horizon looks bright. Here are a few trends to watch:
- New ligands – Beyond TSPO, compounds targeting COX‑2, P2X7 receptors, and even astrocyte markers are in development, expanding the toolbox for molecular imaging inflammation.
- Artificial‑intelligence analysis – Machine‑learning algorithms can automate ROI selection and predict disease trajectories from raw PET data.
- Theranostics – Imagine a tracer that not only lights up inflammation but also carries a therapeutic payload, delivering drugs directly to the inflamed spot.
These advances could turn neuroinflammation PET from a diagnostic curiosity into a routine part of personalized neurology.
Conclusion
To sum it up, a neuroinflammation PET scan gives doctors a unique, non‑invasive window into the brain’s immune activity. It shines a light on conditions where inflammation is a hidden driver, helps tailor treatments, and can even track how well a therapy works over time. While there are legitimate concerns about radiation, cost, and tracer availability, the benefits often outweigh the drawbacks—especially when a clear clinical question needs answering.
If you’re considering a scan, talk openly with your healthcare team about the specific tracer, what the results could mean for your care plan, and any preparations you’ll need. And remember, the field is evolving fast; staying informed means you’ll be at the forefront of cutting‑edge care.
What’s your experience with neuroinflammation imaging? Have you or a loved one taken a PET scan and learned something surprising? Feel free to share—knowledge grows when we discuss it together.





















Leave a Reply
You must be logged in to post a comment.