Ever wondered why doctors sometimes order a “brain scan” and what exactly they’re looking for? In plain language, neuroimaging techniques are the high‑tech lenses that let us peek inside our heads without a single incision. Whether you’re trying to understand a lingering headache, planning a research project, or simply satisfying a curious mind, knowing the strengths, limits, and safety of each scan can turn confusion into confidence.
Why It Matters
First off, let’s answer the most pressing question: what can a brain scan tell you? Think of the brain as a bustling city. Some techniques map the city’s streets and buildings (the structure), while others track traffic flow and power use (the function). When a neurologist orders a scan, they’re usually hunting for one of three things: an abnormal structure (like a tumor), irregular activity (such as a seizure focus), or a metabolic change (like early Alzheimer’s). Knowing which tool fits the job helps you avoid unnecessary appointments, radiation exposure, and the dreaded “waiting‑room anxiety.”
From a personal perspective, I once accompanied a friend to a PET scan for a family history of Parkinson’s. Watching the colorful glow of dopamine‑tracking tracers on the monitor was like seeing a night‑time city map light up. It not only reassured us about his health but also sparked a deeper conversation about how each scan paints a different piece of the neurological puzzle.
Imaging Categories
Neuroimaging broadly splits into three families: structural, functional, and hybrid/emerging techniques. Structural imaging captures the brain’s anatomy—think of it as a high‑resolution photograph of a skyline. Functional imaging reveals how different regions light up when you think, speak, or feel. Hybrid methods marry the two, offering a more complete story.
| Category | What It Shows | Typical Uses |
|---|---|---|
| Structural | Gray‑matter thickness, lesions, bone, fluid | Stroke detection, tumor mapping, trauma assessment |
| Functional | Blood flow, metabolism, electrical activity | Research on cognition, epilepsy localization, psychiatric evaluation |
| Hybrid/Emerging | Combined anatomy + activity + connectivity | Precision surgery planning, advanced research |
Core Modalities
MRI – The All‑Rounder
Magnetic Resonance Imaging (MRI) is the workhorse of modern neuroimaging. It uses powerful magnets and radio waves to create detailed pictures of the brain’s soft tissue, all without ionising radiation. Within the MRI family there are several sub‑types worth knowing:
- Structural MRI (T1/T2, FLAIR) – the go‑to for spotting tumors, demyelination, or chronic lesions.
- Diffusion Tensor Imaging (DTI) – traces the microscopic highways of white‑matter fibers. If you’ve ever wondered how scientists visualize nerve fiber pathways, DTI is the answer.
- Functional MRI (fMRI) – measures the blood‑oxygen‑level‑dependent (BOLD) effect, a subtle shift in magnetic properties when oxygenated blood rushes into an active brain region. According to Oxford’s fMRI introduction, the BOLD signal lets us infer neuronal activity without touching the brain.
Pros: exquisite spatial resolution (down to a millimetre), no radiation, versatile for many disorders. Cons: expensive, noisy, can be uncomfortable for claustrophobic patients, and not ideal for people with certain implants.
PET – The Metabolic Detective
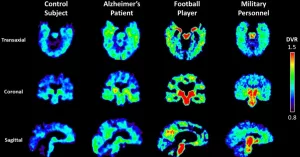
Positron Emission Tomography (PET) works a bit like a biochemical spy. A tiny amount of radioactive tracer—often fluorodeoxyglucose (FDG) for glucose metabolism—travels through the bloodstream. The scanner detects the emitted positrons, producing a colour‑coded map of metabolic hotspots. This is priceless for conditions where function outpaces structure, such as early Alzheimer’s (lower metabolism in the temporoparietal cortex) or certain cancers.
Benefits include unparalleled sensitivity to biochemical changes, but the downside is exposure to low‑dose radiation and the need for a cyclotron‑produced tracer, which can limit availability.
EEG – The Lightning‑Fast Listener
Electroencephalography (EEG) records the brain’s electrical chatter via electrodes on the scalp. It captures activity in milliseconds—far faster than MRI or PET. That speed makes EEG the gold standard for diagnosing seizures, sleep disorders, and for research that needs real‑time feedback, such as brain‑computer interface studies.
The trade‑off? Spatial resolution is modest; you know when something happened but not exactly where. That’s why many labs now pair EEG with MRI to pinpoint the source of abnormal waves.
CT – The Rapid Responder
Computed Tomography (CT) uses X‑rays to create cross‑sectional images of the head within seconds. It’s the first line for acute head trauma, subarachnoid haemorrhage, or when a patient can’t tolerate the longer MRI scan. While its detail is lower than MRI for soft tissue, its speed and widespread availability make it essential in emergency rooms.
Emerging & Hybrid Techniques
Science never sleeps, and neither do neuroimaging innovators. A few exciting developments include:
- PET‑MRI – simultaneously captures metabolism (PET) and anatomy (MRI), delivering a single, richly detailed dataset.
- Functional Ultrasound (fUS) – a portable method that visualises real‑time blood flow, currently shining in animal research and early human trials.
- 7‑Tesla MRI – ultra‑high field scanners that resolve cortical layers you’d normally need a microscope for.
- 3‑D Brain Connectivity Mapping – advanced tractography algorithms stitch together DTI data into immersive three‑dimensional models. Curious? Check out the 3D brain connections guide for a deeper dive.
Benefits & Risks
Every medical test carries a balance sheet of pros and cons. Let’s break it down:
| Technique | Key Benefit | Primary Risk |
|---|---|---|
| MRI | High spatial detail, no ionising radiation | Claustrophobia, metal implant restrictions |
| PET | Metabolic insight, early disease detection | Radiation exposure, tracer availability |
| EEG | Millisecond timing, bedside-friendly | Limited spatial resolution |
| CT | Speed, excellent for acute bleed | Radiation dose (higher than MRI) |
Guidelines from the American College of Radiology recommend choosing the lowest‑dose method that still answers the clinical question. In practice, that means a CT for a sudden head injury, an MRI for chronic pain work‑ups, and a PET when metabolic clues are crucial.
Choosing a Scan
Imagine you’re at a crossroads with three signposts: “Headache,” “Memory loss,” and “Seizure suspicion.” Which direction do you take? Here’s a quick decision matrix to help you and your doctor decide:
| Scenario | Suggested Modality | Why It Fits |
|---|---|---|
| Sudden, severe headache (possible bleed) | CT | Fast detection of blood, easy access in emergency rooms |
| Progressive memory decline | MRI + FDG‑PET | Structural detail plus metabolic patterns typical of Alzheimer’s |
| Unexplained seizures | EEG + MRI | EEG identifies electrical focus; MRI shows anatomical correlate |
| Research on brain networks | fMRI + DTI + 3‑D tractography | Combines functional activation with white‑matter pathways |
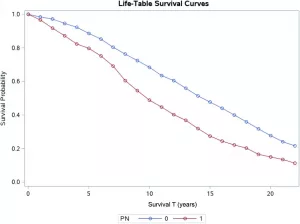
In a recent case study, a 57‑year‑old with early‑onset Alzheimer’s underwent an FDG‑PET that revealed reduced glucose uptake in the posterior cingulate, while an MRI confirmed mild hippocampal atrophy. The combined evidence steered treatment toward cholinesterase inhibitors sooner than it would have otherwise.
Future Trends
What’s on the horizon? A few trends are already reshaping the field:
- Artificial Intelligence – deep‑learning algorithms now flag subtle lesions faster than many radiologists, reducing false‑positive rates and freeing clinicians for patient‑focused care.
- Ultra‑High‑Field 7 T MRI – offers sub‑millimetre resolution, enabling researchers to visualise cortical columns and tiny nuclei previously invisible at 3 T.
- Portable Brain‑Scanning Devices – wearable EEG‑fNIRS combos are being piloted in intensive care units, promising real‑time monitoring without moving the patient.
- Personalised Imaging Pipelines – integrating genetics, lifestyle data, and imaging into a single “digital twin” of the brain, ushering in truly customised treatment plans.
These advances aren’t just tech for tech’s sake; they aim to make scans safer, faster, and more informative for people like you and me.
Conclusion
Neuroimaging techniques are the windows through which medicine and science glimpse the living brain. From the structural clarity of MRI to the metabolic revelations of PET, from the lightning‑fast whispers captured by EEG to the rapid emergency insights of CT, each modality has a unique story to tell. Understanding their benefits, limitations, and appropriate applications empowers you to ask better questions, make informed decisions, and feel more at ease during the diagnostic journey.
If you’re curious about how these scans intersect with other cutting‑edge topics, explore our articles on brain neuroimaging, dive into the world of nerve fiber imaging, or see how nerve fiber pathways shape cognition. Knowledge is the best medicine—so keep asking, keep learning, and feel confident that you’re equipped with the right tools to understand your brain’s amazing inner universe.






















Leave a Reply
You must be logged in to post a comment.