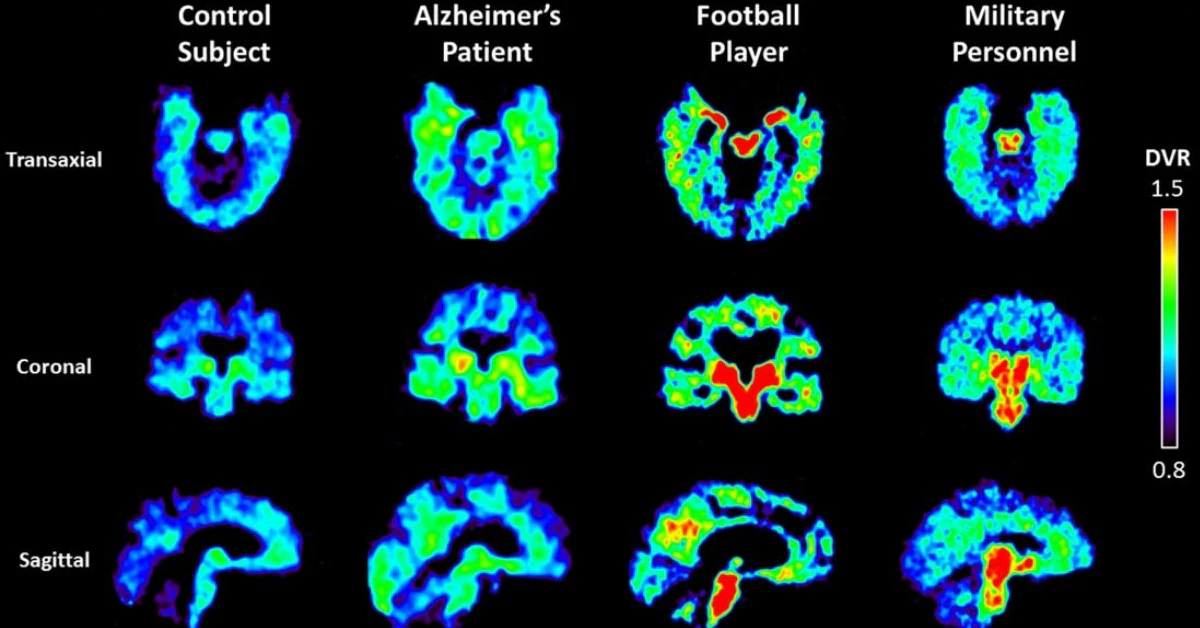
They say the brain is the final frontier, but here’s the thing—we’re finally getting tools that let us navigate that murky terrain of brain inflammation prettymuch like explorers with a flashlight. Imagine having your own pair of X-ray glasses that let you peek inside your brain and spot inflammation in action. Well, buckle up… because that’s exactly where modern PET tracers are headed.
If you or someone you care for has ever wrestled with unexplained neurological symptoms—whether it’s memory fog, MS flare-ups, or Parkinson’s challenges—this matters. But we’re not just talking about “seeing” the brain. We’re talking about seeing what’s happening in it. That’s where the concept of a PET tracer brain inflammation imaging comes into play.
From Glucose Gluttony to Targeted Signaling
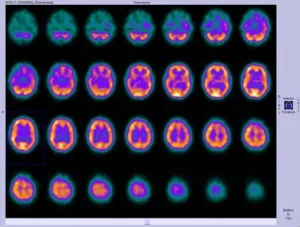
Let me take you back to 1990… no, not your grungy flannel-wearing glory days. This was when FDG PET scans started highlighting brain tumors based on their glucose metabolism like glowing fire signs. But here’s the rub: high glucose uptake doesn’t always scream inflammation.
Flash forward to 2010, and things got real interesting with TSPO tracers. These little guys zeroed in on activated immune cells, specifically microglia and astrocytes, which yell “red alert!” when your brain’s under stress. Yeah, they were a breakthrough. But let’s keep it real—are they flawless? Nope. Genetic quirks can mess up their signal. Like the equivalent of poor WiFi reception.
Enter 2024-2025. Now, we’ve got PET tracer brain inflammation tools that walk into a sci-fi movie. Things like [18F]-T-401 and [11C]-MC1. Why does that matter? Let’s keep this simple: we’re not just guessing anymore. We’re actually seeing inflammation flicker and map it across the brain with more detail—and precision—than ever before. You can almost hear it saying, “Look, I’m doing something important in here!”
Meet the New Kids on the Block
Okay, quick pop quiz: what do [18F]-LW223, [9F]-PDE-1905, and [11C]-MC1 have in common? If you guessed “they’re brain imaging tracers with killer specs,” you’d be right. Let’s crack these open in human-speak:
- [18F]-LW223: Works even if you’ve got genetic code that scoffs at older tracers. No more “Hey, this one doesn’t like you.”
- [9F]-PDE-1905: Goes straight for the microglial activation—the brain’s cranky sentinels. Smoother image, fewer hiccups.
- [11C]-MC1: Locks onto the COX-2 enzyme like a laser-guided handshake. Handy for researchers (and eventually doctors) to track neuroinflammatory processes without guesswork.
If this sounds like alphabet soup cooked in a lab, that’s the point. These tracers aren’t just science fiction—they’re now saving researchers weeks of manual decoding. A recent article explains how [11C]-MC1 is already producing sharper action maps in human studies. Meanwhile, [18F]-Flortaucipir, originally for tau protein in Alzheimer’s, helps connect inflammation dots in dementia care. Real messy, but real useful.
The Brain’s Wild Stress Response
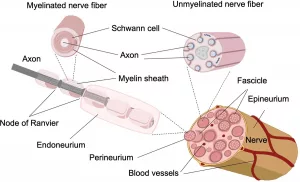
Let’s zoom out for a second. Brain inflammation—aka neuroinflammation—is like a home security system gone too far. Microglia and astrocytes (your brain’s bouncers) jump in to protect you… but sometimes they don’t tap the brakes when things calm down. Understand—not exactly a textbook metaphor… but you get the idea.
How a PET Tracer Turns Stress into Data
Come on, we’ve all had days when our head feels like it’s been hit by a sledge. But picture a scan actually locating where stress in the brain turns into inflammation at the molecular level. It’s not, like… dramatic. It’s outsized.
The nitty-gritty’s not as complicated as it sounds: the 18F or 11C tag in the tracer attaches to proteins like TSPO or MAGL found on inflamed cells. The PET scanner captures tomography snapshots—kinda like a photo album of your brain’s “hot spots.” Think of it as a spotlight falling on troublemakers. According to a paper from Technology Networks, this has opened the door for evaluating neuroinflammation in Alzheimer’s, Parkinson’s, and even depression. Freaky cool, huh?
Real-World Wins You’ll Care About
Let’s get honest. You’re probably here because of a story—yours or someone else’s. Maybe you’ve watched a grandparent spiral into Alzheimer’s, or you’re wrestling with MS wondering why’s this flare-up so darn unpredictable?
Here’s where imaging shines: subtle changes that traditional MRI misses. Science says that [11C]-3F4AP—a myelin-focused tracer—uncovered inflammation in MS patients that wasn’t obvious through symptoms alone. Houston Methodist researchers also saw a clear connection between inflammatory activity and tau buildup in Alzheimer’s, which could lead to earlier interventions. Mind. Blown.
| Tracer | Target | Strengths |
|---|---|---|
| [11C]-PK11195 | TSPO | Early adapter, but inconsistent due to genetics |
| [11C]-MC1 | COX-2 enzyme | First-in-human tracers for specific inflammatory mapping |
| [9F]-PDE-1905 | Phosphodiesterase 4B | Microglia-specific & greater image clarity |
| [18F]-LW223 | TSPO (genetic-insensitive version) | Accurate across genetic types |
Challenges You Should Know: It’s Not Rainbows and Glial Cells
Hold up. Just because something’s futuristic doesn’t mean it’s perfect. In fact, the road to better neuroimaging is unfolding quicker than we can press “print.” But challenges still tower like molasses in January.
The Problem of “Bad Glue”—a.k.a. Nonspecific Binding
You don’t get 100% accuracy with most older tracers. Early TSPO tracers didn’t just bind inflammation—they latched onto any old molecule that’d fool ’em. Hence the “photo album” sometimes caught dull or fuzzy images. Like trying to take a glamour shot through a foggy window.
New tech fixed some, but still—we’re not outta the woods yet. According to analysis from PMC, the confusions don’t stop there. “Suboptimal cellular specificity” …fancy terms, but what it means is this: even top imaging struggles to say, “Hey, that’s microglial flare, not astrocyte-spam.” Yeah. Still gotta tidy those fine lines.
The Genetic Wild Card
Here’s where tech turns quirky. Second-gen TSPO tracers act hella sensitive to genetic differences in users. Think of it like wine—some people don’t get the finer notes, and genetics can impair interpretation. That’s why newer versions like [18F]-LW223 are winning the popularity contest right now—they’re sturdy, even when strapped to genetic variability.
But are we clear sailing now? Not quite.Cue-in the biggest problem of all: most tracers still give us a “yes, there’s inflammation” without handing over the expressway to “why is it happening” files. Science (eventually) will. But here’s where it gets tricky…
Radiation & Cost—Is It Worth the Risk?
Here’s a delicate area: radiation. PET scans use radioactive parts—no getting around that. However, modern iterations like [11C]-MC1 use smaller doses and linger less in the body, which means you’re exposed to minimal stress factors. Still… even those can be a “for research use only” situation. Not exactly weekend hobby stuff.
And the price tag? Cold blood: even routine MRIs strain some budgets. PET? More like a forensic-level money grab.
Drawing the Curtain on What’s Next
Alright. We’ve peeled back the layers. Tracers have come a long way. But what’s next on the horizon for brain imaging that actually makes a dent in healthcare?
Brain Health Beyond Disease Monitoring
Today’s use centers on diseases—Alzheimer’s, Parkinson’s, MS, etc. But what happens when the tech’s advanced enough to monitor inflammation in everyday brain changes?
Johns Hopkins researchers hinted that TSPO tracers could track brain inflammation in post-Lyme disease, where patients report cognitive issues without visible signals before. So what if the playbook expands—to chronic fatigue syndrome? Depression? PTSD?
It’s scifi for now. But people are chasing that trail. Let’s cut through the noise: better tools will one day let us talk to the brain like old friends. “Oh, looks like your inflammation level in that region spiked last month—what were you doing?”
The Connection to You (Even if You’re “Healthy”)
Look, a lot of this rag is aimed at disease, but think ahead: maybe you’re into peak performance. For brainy stuff like that, understanding inflammation before it backfires makes a ton of sense. Inflammation’s a known aggro for mental fatigue, and imaging isn’t just for those jumping through hoops of major neurology studies.
If you’re battling “the Monday blues” that won’t quit… or your brain just won’t turn off even when it should, future imaging tools may offer insight into why. It’s early. But you should care. Here’s why:
- Even slight increases in brain inflammation impact mental clarity.
- Mood disorders like depression may hide underlying inflammation markers that affect treatment outcomes.
- Preventive monitoring might one day give you power over your own neurochemistry (no lab coat required).
The Not-So-Very-Romantic (But Necessary) Realities
Let’s not sugarcoat it—PET imaging brain inflammation doesn’t zoom us straight into “quick fixes.” The tech stretches advanced science… and some hurdles still need punch-before widespread use rolls in.
Biggest gripes so far? SNMMI researchers point to two key issues: signal consistency and cost. Right now, only specialized centers offer imaging, and for rare tracers, the gates stay practically locked. It’s like trying to rent the Nutella of brain imaging—top shelf, but not every pantry carries it.
But hey—progress matters. [11C]-MC1 and [9F]-PDE-1905 are already blowing doors open in human studies. And according to a recent review from Frontiers in Immunology, the fine-tuning is in motion. Real slow, but real meaningful.
So, what’s next? Maybe access issues older tracers face? Maybe a new generation not bound by these limits? Either way, we’ve got momentum.
Failure vs Progress
PET imaging brain inflammation is one of those “try harder” ideas. Even the 2025 advancements come swinging with restrictions. Here are the dang problem areas that try science’s patience:
- Murky enzyme origins: Tracers target specific proteins, but decoding exactly which immune cells crank ’em out still flummoxes scientists.
- Blood-brain barrier blues: Some tracers can’t see through the brain’s firewall without going in sideways and yelling, “I’m through!”
- Financial fog: Even with lower doses, production costs keep these outta everyday diagnostics. Dang.
Still, every one of these roadblocks is like climbing a mountain—wearier legs today, but clearer horizons tomorrow. As one article put it, it’s not about “treatment of the future,” it’s anchoring the science we have what we see—including when inflammation is driving your brain’s chaos bus.
Final Thoughts: The Power—and Complexities—of Knowing What Ails You
PET tracer brain inflammation-specific solutions aren’t just for neurology conferences and research cells in labs. They’re for your cousin with Alzheimer’s staring off at the dinner table, for your friend with MS who’s wrung out after a flare-up, maybe even for you—deep-fried after 90% of recovery from something no one diagnostics properly catches.
This story? It’s not “why sci’s awesome.” It’s “why knowlege can be your armor.” With [11C]-MC1 and [9F]-PDE-1905 in clinics as of 2025, we’re getting better at turning “how bad do I feel?” into data that tells TRUE stories. Not janky guesses.
Still, it’s something you should understand, not something you’ll do tomorrow. PET tracers are a tool with boundaries we now speak to—something doctors haven’t always had. Prior to 1990, FDG scans (based on sugar uptake) could only answer “weird glow” as “maybe epilepsy, maybe tumor, maybe inflammation.” Bleh. Now? Specificity’s climbing inch by inch. But guess what: the steady climb forward’s lead by us—that’s all of us, immune of worrying about how cozy our brains feel. Brain inflammation has the spotlight. And better tools will follow.
Let’s leave you with this: would knowing your inflammation activity change your diet, your stress routine, or even your doctor’s path? Maybe. Or maybe you’ll think, “Yeah, I want that pano of my brain’s party someday.”
Feel Like an Expert Yet?
We told you this isn’t just announcing jargon—that’s storytelling with data. You don’t need to get a PhD to follow the beat. You only need to give a dentch.
Or maybe you’re thinking, “But how do I get one of these scans right now?” Smart question. The short answer? Ask your neuro or imaging center if they’re using probes like [9F]-PDE-1905; it’s a good foot in the door.
The longer answer? Science is still unpacking the clinical kinks. But guess what? You’re early enough in the saga to actually watch the next episode.
- Timelines of tracer adoption should dig creep into mainstream neurology over the next decade
- Applications will open beyond disease imaging into behavioral and lifestyle domains
- And yes – the field will probably lament how long we dragged our heals once we’ve got it
So, what now? If you’ve got questions (or a nonchalant “this han’t happened to me… yet”), drop them below.
Honestly, the more people know the brutal truths and the eventual wins—the better we all grapple with brain health. And wouldn’t it mean something powerful having that conversation—someone uncertain about their foggy mind—gets a new kind of T*Ruth via a PET scan? Oh yeah. It would. Because the point isn’t just finding inflammation. It’s handling it—your way. Science spends time defini fatt—and maybe we’ll make the next blog: “How to Talk to Your Doctor About Brain Imaging.”
Stay curious. Stay persistent. And keep your brain’s burning bush in check.




















Leave a Reply
You must be logged in to post a comment.