Ever wonder why your heart starts pounding the moment you hear a sudden car horn? That rush is your sympathetic nervous system in action – the part of your body that flips the “go” switch when danger or stress shows up. In a nutshell, the sympathetic nervous system function is to accelerate the heart, open up your airways, dilate pupils, release glucose, and temporarily slow digestion so you can think and act quickly.
But here’s the twist: the same system that saves you from a falling tree can also keep you on high alert long after the threat has vanished. Prolonged activation can lead to hypertension, anxiety, and even metabolic trouble. Knowing how this system works helps you enjoy its benefits while keeping the risks in check. Let’s dive in together, friend‑to‑friend, and unpack the science, the signs, and the simple habits that keep the balance right where it should be.
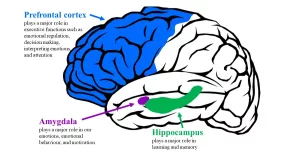
Core Anatomy
Spinal‑Cord Origins
The sympathetic nervous system (SNS) kicks off in the thoracolumbar region of your spinal cord, specifically between the T1 and L2 vertebrae. These tiny nerve cells sit in the lateral horns, also called the intermediolateral column. That spot is the launchpad for every “fight‑or‑flight” signal your brain sends.
According to a StatPearls chapter on neuroanatomy, the pre‑ganglionic neurons arise from these spinal segments and travel out through the ventral roots before joining the sympathetic chain [1].
Diagram suggestion
Imagine a vertical slice of the spinal cord: the grey matter forms a “C” shape, and the lateral horns stick out like tiny side‑branches. That’s where the SNS gets its spark.
Key Pathways & Ganglia
From the spinal cord, the pre‑ganglionic fibers either synapse in the paravertebral chain (the “sympathetic trunk”) or hop over to the pre‑vertebral (collateral) ganglia near the abdominal aorta. Post‑ganglionic fibers then hitch a ride on blood vessels to reach their target organs – the heart, lungs, eyes, skin, and more.
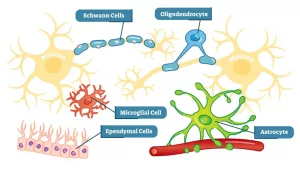
Neurotransmitters & Hormones
- Acetylcholine – released by pre‑ganglionic neurons to activate the ganglia.
- Norepinephrine – the main messenger for post‑ganglionic fibers, tightening blood vessels and boosting heart rate.
- Epinephrine (adrenaline) – secreted by the adrenal medulla into the bloodstream, creating a body‑wide “go” signal.
What the SNS Actually Does
Quick‑Start Fight‑or‑Flight Actions
When danger looms, the SNS flips several switches at once:
Heart
Your heart beats faster and stronger, pumping oxygen‑rich blood to muscles. WebMD notes that this increase in cardiac output is one of the hallmark signs of sympathetic activation [2].
Lungs
Bronchi dilate, letting more air in so your muscles get the oxygen they crave. Your breathing rate climbs, a sensation most of us recognize as “short‑of‑breath” during a panic moment.
Eyes
Pupils widen, letting in extra light and sharpening visual acuity. Ever notice how you see more clearly when something startling happens? That’s your sympathetic nervous system at work.
Metabolic Mobilization
The liver receives a signal to break down glycogen, flooding the bloodstream with glucose. Fat cells also release fatty acids for an extra energy boost. This rapid fuel surge is why you feel a sudden surge of strength when you need to sprint away.
Resource Redistribution (What Gets Paused)
While the SNS revs up your engine, it simultaneously presses the “pause” button on non‑essential functions:
- Digestion – peristalsis slows, and stomach acid production drops.
- Urinary & reproductive systems – activity is temporarily suppressed.
This trade‑off conserves energy for the muscles and brain, the two organs that matter most in an emergency.
Hormonal Cascade & the Adrenal Medulla
The sympathetic nervous system talks to the adrenal glands, prompting them to dump epinephrine and norepinephrine straight into the bloodstream. Britannica explains that this “sympatho‑adrenal” response amplifies the fight‑or‑flight effect across the whole body [3].
Beyond Stress: Exercise, Illness & Immunity
Even a good workout triggers sympathetic activation, but only for a short burst. During a fever, the SNS helps raise body temperature and mobilize immune cells. So, not every spike is a problem – context matters.
Stress & the SNS: When “Too Much” Becomes a Problem
Chronic Activation & Health Risks
When the SNS stays switched on day after day, the body pays a price. Chronic catecholamine exposure can push blood pressure up, spike blood sugar, and wear down the cardiovascular system. Britannica links long‑term stress‑induced SNS activity to hypertension, hyperglycemia, and even type‑2 diabetes [3].
Signs You’re Over‑Activated
Do any of these sound familiar?
- Heart racing at the thought of a meeting.
- Insomnia or restless sleep.
- Frequent stomachaches or “butterflies” that never go away.
- Excessive sweating, even when it’s not hot.
If you tick several boxes, your sympathetic nervous system stress response may be stuck in the “on” position.
Balancing the Autonomic Scale
| Feature | Sympathetic (SNS) | Parasympathetic (PNS) |
|---|---|---|
| Main Role | Prepare body for rapid action (“fight‑or‑flight”) | Restore calm and conserve energy (“rest‑and‑digest”) |
| Primary Neurotransmitter | Norepinephrine | Acetylcholine |
| Heart Effect | Increases rate & force | Decreases rate & promotes relaxation |
| Digestive Effect | Suppression | Stimulation |
| Typical Activation Time | Seconds (instant) | Minutes to hours (gradual) |
Evidence‑Based Strategies to Calm the SNS
Good news: you can train your nervous system to hit the reset button more often.
- Breath work – Slow diaphragmatic breathing (4‑2‑4 pattern) lowers norepinephrine levels within minutes.
- Progressive muscle relaxation – Tensing then releasing each muscle group signals the brain that danger has passed.
- Regular aerobic exercise – Moderate‑intensity cardio improves heart‑rate variability (HRV), a reliable marker of autonomic balance (see a 2023 Journal of Psychophysiology study).
- Mind‑body practices – Yoga, meditation, or tai chi activate the parasympathetic branch.
Real‑World Applications & Everyday Examples
Case Study 1 – The Runner’s Rush
Imagine you’re sprinting the last 200 meters of a 5 k race. Your SNS fires up, sending a surge of adrenaline, pumping blood to leg muscles, widening airways, and sharpening focus. After you cross the finish line, the parasympathetic system gently lowers the heart rate, allowing you to catch your breath and recover. This back‑and‑forth is a perfect illustration of how the two systems cooperate.
Case Study 2 – Stress at the Office
Picture a looming deadline. Your brain labels the situation as a threat, and the sympathetic nervous system spikes: heart thumps, palms sweat, thoughts race. If the pressure lingers for weeks, those spikes become a steady hum, nudging blood pressure upward and making you prone to anxiety. Introducing a 5‑minute breathing break each afternoon can reset the balance and keep the “stress soundtrack” from becoming background noise.
Practical Checklist for Daily Balance
Here’s a quick, friendly cheat‑sheet you can stick on your fridge:
- Take three deep breaths before checking your phone in the morning.
- Move your body for at least 20 minutes a day – even a brisk walk counts.
- Stay hydrated; dehydration can amplify sympathetic signals.
- Prioritize 7‑9 hours of sleep; sleep deprivation fuels chronic SNS activation.
- Schedule a “digital sunset” – turn off screens at least an hour before bed.
Mini‑FAQ Nuggets (Featured Snippets)
What triggers the sympathetic nervous system? Anything your brain perceives as a threat or demand – a loud noise, a stressful thought, intense exercise, or even caffeine.
Can I train my SNS to be less reactive? Absolutely. Regular breath work, meditation, and balanced exercise all teach the nervous system that most “threats” are safe, reducing over‑reactivity.
Is the SNS always “on”? No. It operates at a low basal level to maintain homeostasis, then ramps up when needed and hands control back to the parasympathetic system afterward.
How Professionals Evaluate SNS Function
Clinical Tests & Measurements
Doctors have a toolbox for checking sympathetic tone:
- Heart‑rate variability (HRV) – Higher variability usually means a healthier balance.
- Plasma catecholamine levels – Blood tests can reveal elevated adrenaline or norepinephrine.
When to Seek Medical Advice
If you notice persistent tachycardia, unexplained high blood pressure, chronic anxiety, or digestive disturbances that don’t improve with lifestyle tweaks, it’s time to talk to a healthcare professional. Early intervention can prevent long‑term complications.
Potential Treatments & Interventions
Beyond lifestyle changes, clinicians may prescribe:
- Beta‑blockers – Medications that blunt the heart’s response to norepinephrine.
- Biofeedback – Training you to see and control physiological signals in real time.
- Cognitive‑behavioral therapy (CBT) – Helps reframe the mental triggers that launch the SNS.
Conclusion
Understanding sympathetic nervous system function is like getting the user manual for your body’s built‑in emergency response. It powers the quick bursts of energy that let you dodge a car, ace a presentation, or finish a tough workout. Yet, when the system stays stuck in “high gear,” the same mechanisms contribute to hypertension, anxiety, and metabolic issues.
By recognizing the signs of chronic activation and using simple, evidence‑backed tools—deep breaths, regular movement, and moments of calm—you can enjoy the protective benefits of the SNS without paying the hidden health costs. Remember, your nervous system is adaptable; you have the power to train it toward balance.
What’s one small habit you’ll try today to keep your “fight‑or‑flight” in check? Drop a comment below, share your experiences, or sign up for our weekly “Balanced Autonomic Living” newsletter. Let’s navigate this journey together.



















Leave a Reply
You must be logged in to post a comment.