Hey there, future mom (or dad‑to‑be)! Let’s cut to the chase: you’ve probably heard the words “cholesterol” and “progesterone” tossed around at your prenatal visit, and you might be wondering why they matter together. The short answer? They’re a dynamic duo that fuels your baby’s growth, keeps your uterus ready for implantation, and even helps protect you from infections. In the next few minutes we’ll break down the science, the risks, and the simple things you can do to keep both in a healthy balance.
Quick Answer
What they are: Cholesterol is the fatty molecule that serves as the raw material for many hormones, including progesterone. Progesterone is the steroid hormone that tells your uterine lining to stay thick and vascular, which is crucial for a successful pregnancy.
Why they matter together: Your liver ramps up cholesterol production by 30‑40 % during pregnancy to give the placenta enough building blocks for progesterone. Progesterone, in turn, modulates your immune system and even nudges cholesterol levels down a notch when it’s most needed.
Bottom‑line: Maintaining a healthy range for both cholesterol and progesterone helps lower miscarriage risk, supports fetal development, and promotes overall prenatal health. Simple monitoring and lifestyle tweaks can make a big difference.
Science Link
Let’s dive a little deeper—no heavy textbooks, just the basics you need to feel confident.
1. Cholesterol as the building block for steroid hormones
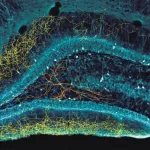
Every steroid hormone, from estrogen to cortisol, starts its life as cholesterol. The journey goes like this: cholesterol → pregnenolone → progesterone (and then on to other hormones). This pathway happens in the ovaries, placenta, and even in the brain. Healthline explains it in plain English, noting that the liver makes cholesterol, which travels around the body on lipoproteins (LDL and HDL).
2. Placental uptake of LDL and progesterone output
Scientists have actually grown human placental cells in the lab and watched how they react to different lipoproteins. When they fed the cells low‑density lipoprotein (LDL)—the “bad” cholesterol—they saw progesterone secretion jump from roughly 100 ng/mg protein to almost 400 ng/mg at the highest LDL dose. High‑density lipoprotein (HDL) also boosted progesterone, but only about half as much as LDL.
| LDL (µg protein/mL) | Progesterone Secretion (ng/mg protein) |
|---|---|
| 0 | 100‑190 |
| 210 | 250‑300 |
| 420 | ≈ 390 |
This tells us that a healthy rise in LDL during pregnancy isn’t a problem—it actually fuels the hormone that keeps your uterus ready for baby.
3. Why cholesterol spikes in pregnancy
During the first trimester your body is building new blood vessels, making cell membranes for the growing fetus, and synthesizing hormones. All of those tasks need cholesterol, so your liver steps up production. The result? A modest but consistent increase in total cholesterol, especially the LDL fraction, which is perfectly normal and even beneficial. Healthline notes this 30‑40 % rise helps ensure there’s enough material for progesterone and vitamin D production.
Progesterone Role
1. Preparing the uterine lining
Progesterone tells the endometrium (“lining of the uterus”) to thicken, become more vascular, and secrete nutrients. Think of it as the “cozy blanket” that keeps the freshly implanted embryo warm and well‑supplied. Without enough progesterone, the lining can break down early, leading to spotting or even a miscarriage.
2. Immune modulation & infection protection
Pregnancy is a bit of an immunological paradox: you need to tolerate the semi‑foreign fetus while still defending against pathogens. Progesterone helps calm the immune response, preventing the body from rejecting the baby. The trade‑off? A slightly higher susceptibility to infections in the first trimester. Interestingly, progesterone’s dip in cholesterol at its peak may actually be a protective adaptation—many viruses and bacteria need cholesterol to enter cells, so lowering cholesterol can limit their foothold. A 2013 study describes this “second‑order adaptation”.
3. Timing: luteal phase, first trimester, and beyond
The corpus luteum (the structure that forms from the follicle after ovulation) pumps out about 40 mg of progesterone each day in early pregnancy. By week 8‑10, the placenta takes over, producing even higher levels to sustain the growing fetus.
4. Signs of low progesterone
If progesterone falls short, you might notice:
- Unexplained spotting or light bleeding
- Cramping that feels “off‑beat” with normal period pains
- Difficulty conceiving after multiple cycles (known as luteal phase deficiency)
These symptoms don’t guarantee a problem, but they’re worth discussing with your OB‑GYN, especially if you’ve experienced a prior miscarriage.
Benefits & Risks
1. High cholesterol & pregnancy complications
While the normal rise in cholesterol is fine, excessively high levels (especially LDL > 190 mg/dL) have been linked to gestational hypertension and pre‑eclampsia. A large cohort study published in 2022 found that women with LDL above this threshold were 1.5‑times more likely to develop high‑blood‑pressure disorders.
2. Low progesterone & miscarriage risk
Research shows that women with serum progesterone under 10 ng/mL in the first trimester have a significantly higher chance of recurrent miscarriage. Some clinics offer progesterone supplementation (usually in micronized oral or vaginal form) to raise those numbers and improve outcomes.
3. Interplay: When one spikes, the other may dip
Peak progesterone in the first trimester often coincides with a modest dip in LDL. This isn’t a glitch—it’s the body’s way of balancing hormone production while limiting cholesterol‑dependent pathogens. Imagine a seesaw: as progesterone rises, cholesterol gently lowers, keeping the system steady.
4. Safe monitoring strategies
Here’s a practical checklist you can bring to your next prenatal visit:
- Fasting lipid panel each trimester (total cholesterol, LDL, HDL, triglycerides)
- Serum progesterone test at 6‑8 weeks if you’ve had prior loss or fertility concerns
- Ask your provider about ACOG’s 2024 prenatal care recommendations
Lifestyle Tips
1. Nutrition that supports healthy lipids
Eating the right foods can keep your cholesterol in the sweet spot while giving your body the nutrients it needs for hormone synthesis.
- Omega‑3 fatty acids (salmon, sardines, walnuts) boost HDL and reduce inflammation.
- Fiber‑rich fruits and veggies (berries, leafy greens) help lower LDL.
- Swap saturated‑fat heavy foods (fried items, fatty cuts) for lean proteins (chicken, beans).
2. Exercise & stress management
Moderate aerobic activity—think brisk walking, swimming, or prenatal yoga—about 150 minutes per week can raise HDL by up to 10 %. Plus, moving your body releases endorphins that support a balanced endocrine system.
3. Sleep & circadian rhythm
Your hormone factories love regular sleep. Aim for 7‑9 hours nightly; the body’s melatonin surge at night helps convert cholesterol into pregnenolone, the first step toward progesterone.
4. When to consider supplements
Some nutrients are “bonus players”:
- Vitamin D (helps convert cholesterol into hormones) – 600‑800 IU daily is a common prenatal dose.
- DHA (an omega‑3) – 200‑300 mg daily supports both lipid profiles and fetal brain growth.
- Magnesium – can aid in vascular health, especially if you’re prone to high blood pressure.
Always run these by your provider before adding anything.
Bottom Line
Keeping cholesterol and progesterone in harmony is like fine‑tuning a musical duet—each note matters, and together they create the beautiful melody of a healthy pregnancy. Cholesterol provides the raw material, progesterone shapes the uterine environment, and both influence your immune balance and fetal development. By understanding the science, getting the right labs, and embracing simple lifestyle habits, you give yourself and your baby the best possible start.
If you’re unsure where you stand, schedule a quick lab check‑up and chat with your OB‑GYN about a personalized plan. Your body is already doing an amazing job; a little extra knowledge and a few gentle tweaks can make the journey smoother, safer, and more joyful.



















Leave a Reply
You must be logged in to post a comment.