Look, if you’re a woman with PCOS and you’ve ever felt like your body was working against you when trying to get pregnant, you’re not imagining things. The numbers don’t lie: miscarriage rates among women with PCOS hover around 30-50%, triple what most people experience. You read that right—triple.
But here’s something not many doctors tell you upfront—it’s not always about your eggs, those extra months of oviston on Clomid, or even that time you had a yeast infection you swear is never going away. Nope. The ESHRE 2024 Annual Meeting? They dropped a truth bomb: certain gut bugs and metabolic oddities are crashing your odds of a full-term pregnancy like a wrecking ball. Who knew your gut flora played thermostat with your fertility?
Still, don’t panic just yet. We’re peeling back what’s really going on beneath the surface—because yes, your gut matters, but so do your sleep patterns, your diet quirks, and how much Facebook fighting you’ve been doing over birth plans (we’ve all had that late-night comment section rage). Stick around, learn what’s tested, what isn’t, and how you can stack the deck in your favor without needing a PhD.
Your Body’s Hormonal Puzzle Has More Gaps
Know that high testosterone bump you’ve gotten used to? And that insulin spike that hits about three hours after you down your third cupcake in an effort to “feel better” (hey, judgment-free zone here)? Turns out these hormonal misbehavers are partially to blame for your higher-than-average risk of miscarrying.
In fact, a study published in PMC 2023 looked at women aged 25–40 undergoing fertility treatment, and guess what happened? Those with insulin resistance and elevated LH were more likely to crash before week 12. Not every case, but the pattern was loud and clear.
Insulin Gone Rogue: Not Just a Blood Sugar Issue
Why does this happen? Because those stubborn insulin levels? They affect your uterine lining like static electricity messing up your hair. Instead of being soft, responsive, and then baby-friendly, your endometrium jams up, overheats, and basically says “quit looking at me like that” before even thinking about letting an embryo stick.
And it’s not just about rolling bloodwork at your next OB visit (unless you’re doing it after 10 p.m. with jandedo DBA nerves, which we’re all familiar with). Your insulin spikes send shock waves to placental cells, constricting blood flow to your newly-formed embryo. Real. Messy.
Obesity—Not Just a Number
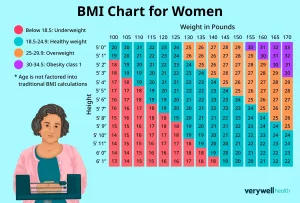
Do yourself a favor: don’t blame yourself for weight gain. The PCOS weight train is a monster, and it doesn’t roll out the moment you take a pregnancy test. But here’s the raw truth—we’ve read studies published in ScienceDirect 2024 where patients with Body Mass Index over 30 had 2x higher miscarriage odds versus their natural-conception counterparts.
Then again, I saw a woman once carrying her third PCOS baby, two tubes tied, zero weight loss. She just focused on her glucose stability and sleep. Long story short: your body is not a math problem. But certain variables? They just matter more than others. Like, way more.
So… Is Recurrent Pregnancy Loss Normal for PCOS?
Not entirely. Some of us penciled in back-to-back 6-week scans only to face the same cold confirmation 3x in a row. A call it “The Groundhog Day of Pregnancy.” But is it just because of PCOS? Maybe, maybe not. A 2023 Fertility Family article dropped something we didn’t expect: yes, PCOS pops up around 40-80% in RPL cases, but so do undiagnosed clotting issues and TSH screks.
Your Gut’s Meta
Now—if your title allowed, you’d be forgiven for thinking gut bacteria was fluff. But here’s the unfiltered: women with moderate to high PCOS symptoms have seen a consistent dysbiosis in their gut. Others have it full of Partium kind of MRSA-like disruptors—bugs that cause low-level inflammation and throw your immune system into “biohazard mode.” This might be why your doc keeps saying: “you look inflamed.”
And it doesn’t stop with IBS-like symptoms. We’re talking about gut health directly influencing amino acid pathways, those same amino acids that nourish the embryo during the first few weeks. It’s like ordering a really complex stir fry and then realizing one ingredient keeps canceling the whole thing. That’s what’s happening here at a metabolic level.
Gut Harmony or Hormonal Breakdown?
Sometimes you have to do the dispersal check. What’s living in your gut might upregulate PAI, lipopolysaccaride binding proteins, and other bio-oddballs that ramp up inflammatory activation.
Clean gut means better messaging between your intestines and your ovaries, less interference where your reproductive system doesn’t need it. Mice studies show that low Lactobacillus concentrations trigger systemic inflammation that’s pure fire.
Even throw a amino acid panel in there. Valine, leucine, isoleucine spikes have been reproducibly high in PCOS patients with repeat losses. Is that a determinant? Possibly.
Metabolic Imbalance Playbook: Real Talk
If your blood work keeps waving yellow flags like high homocysteine, low SHBG, or your leptin levels are on overdrive, your metabolic health is 80% of the solution—20% is survival mode and stress response.
Meet Metformin: The Love-Hate Ally
This is the drug that polarized Reddit threads for years. No doubt, you’ve heard one person say it’s a miracle and another swear they cried over a magnesium deficiency while on it. But in a 2020 study by PERLA Health, metformin reduced miscarriage risk by up to 20% in progesterone-deficient patients.
Does it work for everyone? Nope. Is it just a glucose cop? Not entirely. But if your doctor chucks you on it and you suddenly see some order in your blood sugar chaos, it’s probably the safest bet in a high-stakes game.
Insulin-Free Diet: Parse this
If we lost you during the whole “chronic insulin buzzkill in the first trimester” part—grab your compass. We all crave quick carbs during pregnancy, and you’re not a coward if those cravings hit hard. Especially with PCOS, that’s just your amygdala screaming “give me energy now!
But here’s the insider tip: distribute carb intake across six meals. Instead of “hangover pizza and cereal-based hangover,” try medium-chain fats (grass-fed butter, avocados, maybe toast oil instead of fruit syrup). Your endometrium will get memo that you’re working with it, not against it.
Endometrial “Aging” and What You Can Do
Hold up: We’re not talking about egg age like a decades/current egg leakreacher. Endometrial aging is about your uterine lining aging a decade ahead of schedule in some studies—that’s your inner lining looking like it celebrated its 40th birthday when you haven’t even had your 35th.
So why does it matter if your uterine lining’s on a premature walkout crew? Because glycodelin and IGF-binding proteins take a hit, messing with embryo generosity. It’s like trying to patch flimsy wires with duct tape and hoping everything holds through a storm. Not what you want.
Not All Complications Happen in Week 6
PCOS moms often face what we love to call the 12-week plateau. After that, the battle against gestational diabetes, blood pressure wildcards, and preemies sets in—because apparently, 24 has to do everything
Early Loss, Late Drama
Can’t stress-watch “Euphoria” and have a low-complication pregnancy? You might have to choose. Because though most losses fall before the first trimester mark, later inflammation still complicates things.
Case in point: A 2024 meta-review found PCOS pregnancies carried higher risk of late preterm and Preeclampsia than others. And no, “probably normal” doesn’t cut it when you’ve already gone through the emotional wringer once.
Baby Outcomes With PCOS? Mildly Janky (Sometimes)
| PCOS Pregnancy Risk | General Population Risk |
|---|---|
| SGA (small gestational age) | 8-10% |
| Meconium leakage | 1-2% |
| Low Apgar score | 3-4% |
Does that scare you? It should. But here’s how to take back control: track progress early, ask about Doppler scans around week 28, and keep your glucose within a narrow range. Not perfection. Just management in the low drama zone.
Managing PCOS Before Baby Actually Sticks
Staycation? Instagrammable meal prep? A non-guilty glass of Grenache? Hyperbole, but maybe not.
The actionable stuff before conception includes bread delivered to your doorstep, night-heavy meditation, and basic rest balances. Sleeping 8 hours on a near-empty stomach doesn’t help—hello, poor egg selection. Disregard every anti-PCOS mindset that includes “carb starvation” or 90-minute spin cycles in hopes of cycling pregnancy in. Balance, babes. Breathing into your belly might do more than a 5-day cleanse ever will.
Fertility Treatments vs. Natural Cycles
Alright—if your OB dropped the name IVF, well—read this part twice.
Controlled trials show IVF can offer better outcomes in PCOS patients, especially those with dimorphic conversion and insulin crashes. But with it comes a warmer than usual chance of putting up with a luteal phase rollercoaster. Like, you baby on may spike progesterone drops like a bad Instagram story and you experience a classic “early DECRIS. Does that mean we all need IVF? No. But it’s on the table, for sure.
Dat question mark in your brain: Is your fertility center PCOS-inclusive? If they’re not making special realignments in your triggering, maybe go elsewhere.
Real Experts Understand Your Real Struggle
Final question? What does a meaningful consultation even look like for PCOS? One where you’re not dismissed with *“master your mindset, breathe better,” or the ever-unsettling “Do you really need that glucose monitor? Because it’s not for frilly tea parties.” No—it’s about accuracy, documentation, and matching hormones with each other instead of praying for lightning chemistry.
Red Flags in Doctor Relationships
‘ve done it: Walked into a fertility center rocking your PCOS, only to get hit with a “You should maybe just slim down first.” Clinical facepalm. Because if they’re not running certain panels—show them the door.
Good doctors already know the gut-amino acid link, screen for insulin counting features, and openly track reproductive hematology panels. Others send you off with a vitamin D script and a nod toward the exit. No thanks.
Final Word: You’re Not a Statistical Aberration
Lete you in on a little secret: you’re not doomed to a string of losses. Although PCOS raises odds, the more we peel back the layers the more we realize it’s all junk in the system. Gut microbiomes acting up, metabolic balance with one foot on a cliff, and insulin doing parkour where it shouldn’t even try. Fix just one of these issues with quality medical support and your chances leap.
Still JIC, keep proactive. If your body wants to assimilate back to balance, it’ll show up. Relentless follow-ups matter. Support groups matter even more. Long story short: PCOS doesn’t mean you belly stat bellows out in week 8 and that’s the end of your eat/drink/life-with-responsibility plan. Pregnancy is still possible. Baby bottles, midnight snacks, and a full-term healthy sprint? Real, even for PCOS.
























Leave a Reply
You must be logged in to post a comment.