Hey there, friend. If you’ve landed on this page, you’re probably looking for clear answers about a condition that sounds as intimidating as a thunderstorm in a glass house—severe epileptic encephalopathy. The short answer? It’s a form of epilepsy where the seizures themselves become a silent thief, stealing the brain’s ability to develop normally. The good news is that, with early detection and a tailored plan, we can slow the thief down, keep the lights on, and give families a real sense of hope.
What Is It
In plain language, severe epileptic encephalopathy is an umbrella term for a group of childhood epilepsy syndromes that not only produce frequent, hard‑to‑control seizures but also cause progressive cognitive decline. Imagine a radio that keeps crackling while you try to listen to your favorite song; the crackles (seizures) drown out the melody (normal brain development). The condition is most common in infants and young children, and the electrical storms on EEG often look like “burst‑suppression” or “hypsarrhythmia”—patterns that scream “something’s wrong with the wiring.”
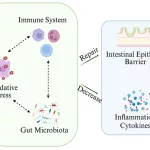
Why does this happen? The brain’s electrical activity, when it’s too chaotic, can actually damage neurons. The concept is backed by the National Center for Biotechnology Information, which notes that “aggressive ictal and electrographic activity during brain maturation is the main cause of progressive cognitive deterioration”according to a 2025 NCBI review. So, the seizures are not just symptoms—they’re part of the disease process.
Why It Happens
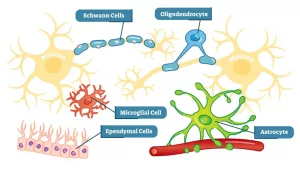
At the heart of many severe cases lies a problem with how neurons move chemicals in and out of the cell—a classic case of a faulty transport protein. One of the most talked‑about culprits is the SLC13A5 gene, which encodes a citrate transporter that fuels the brain’s metabolic engine. When this transporter doesn’t work right, the neuron’s energy supply goes haywire, leading to excess excitation and, ultimately, seizures.
Think of neurons like tiny engines that need the right fuel mixture to run smoothly. If the fuel (citrate) can’t get in, the engine sputters, producing dangerous back‑fires (seizures). This mismatch also messes with the delicate balance of glutamate (excitatory) and GABA (inhibitory), pushing the brain toward an over‑excited state.
Besides SLC13A5, other brain transport proteins—such as the ones that shuttle amino acids, glucose, or ions—can be defective. When they’re out of whack, neuron metabolism (neuron metabolism) falters, and the electrical storm builds.
Researchers in a 2024 Cureus review highlighted that these metabolic errors trigger a cascade: excess glutamate → calcium overload → cell death. It’s a bit like a domino line—once the first piece falls, the rest follow quickly.
How It Looks
When severe epileptic encephalopathy shows up, the first clue is often a seizure pattern that refuses to settle. Parents may notice:
- Sudden, jerky movements (myoclonic jerks) in the first few months of life.
- Stiffening episodes (tonic spasms) that can last several seconds.
- Clusters of seizures that happen back‑to‑back, sometimes lasting minutes.
Alongside these seizures, children often experience a developmental plateau or regression. A baby who was beginning to smile might suddenly lose that ability; a toddler who started crawling could stop progressing. It can feel heartbreaking, but it’s crucial to recognize these red flags early.
One real‑world story that sticks with me is about a little girl named Maya. At three months, her parents heard tiny “clucking” sounds that turned out to be myoclonic jerks. By six months, her EEG showed a classic burst‑suppression pattern, and genetic testing revealed a mutation in the SLC13A5 gene. The diagnosis was a shock, but once the team started a targeted metabolic diet and adjusted her meds, Maya’s seizure frequency dropped dramatically, and she began to regain eye contact—a small victory that meant the world to her family.
Getting Diagnosed
The diagnostic journey is a bit like piecing together a puzzle. Here’s a straightforward roadmap you can share with your doctor:
| Step | What Happens |
|---|---|
| 1️⃣ Clinical History | Detailed seizure description, developmental milestones, family history. |
| 2️⃣ EEG | Captures the characteristic burst‑suppression or hypsarrhythmia patterns. |
| 3️⃣ MRI | Looks for structural brain abnormalities that could be causing the seizures. |
| 4️⃣ Metabolic Screening | Blood and urine tests for abnormal citrate, lactate, or other metabolites. |
| 5️⃣ Genetic Panel | Tests for genes like SLC13A5, STXBP1, SCN2A, among others. |
When the brain transport protein issue is suspected—say, the child has unusually high citrate levels—your doctor will likely prioritize metabolic testing alongside the genetic panel. The International League Against Epilepsy (ILAE) recommends this tiered approach to avoid missing treatable causes1.
Remember, a diagnosis is not the end; it’s the beginning of a personalized plan.
Treating It
There’s no one‑size‑fits‑all medication for severe epileptic encephalopathy, but there are several strategies that together form a comprehensive defense.
Acute Seizure Management
In an emergency, fast‑acting benzodiazepines (like lorazepam) are the go‑to. If a seizure lasts longer than five minutes, call emergency services—time is brain.
Long‑Term Medications
Some anti‑seizure medicines have shown promise in specific sub‑syndromes:
- Stiripentol – often added to valproate for Dravet‑type syndromes.
- Fenfluramine – approved for Dravet and Lennox‑Gastaut, can cut seizure frequency by half.
- Cannabidiol (CBD) – useful in many refractory cases, especially when combined with clobazam.
For children with SLC13A5 epilepsy, the evidence is still emerging, but some families report modest improvement with a ketogenic diet that bypasses the faulty citrate pathway.
Targeted Metabolic Therapies
When the problem is a faulty transport protein affecting citrate, dietary modifications can be a game‑changer. The ketogenic diet—high fat, low carbohydrate—shifts the brain’s fuel source from glucose to ketones, reducing the demand for the broken citrate transporter. Adding citrate supplements under medical supervision may also help, though it’s not a universal fix.
Emerging Disease‑Modifying Approaches
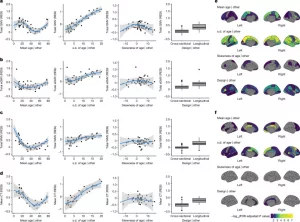
Scientists are tinkering with gene‑therapy vectors and antisense oligonucleotides that silence the mutant gene transcripts. Early‑phase trials for STXBP1 and SLC13A5 are already recruiting participants, offering a glimmer of hope for disease modification rather than just seizure control.
Balancing Risks & Benefits
Every medication comes with side‑effects—weight gain, liver enzymes, behavioral changes. It’s a delicate balance. A handy table can help you and your neurologist weigh pros and cons:
| Medication | Potential Benefit | Common Risks |
|---|---|---|
| Stiripentol | 30‑50% seizure reduction | Fatigue, appetite loss |
| Fenfluramine | Up to 70% reduction | Cardiac valve concerns (monitoring needed) |
| Ketogenic Diet | Improves seizure control in metabolic forms | Constipation, high cholesterol |
| CBD | Seizure frequency drop in many cases | Somnolence, drug interactions |
Always discuss the trade‑offs with your specialist. The goal is to keep seizures low enough that the brain can focus on growth, not on fighting electrical storms.
Living Everyday
Beyond the medical arsenal, families need practical tools to keep daily life as normal as possible.
Home Safety
Secure water tubs, use corner protectors, and keep a rescue medication (like rectal diazepam) within arm’s reach. A quick check: can your child safely bathe without slipping? If not, consider a handheld showerhead.
School & Social Life
Work with the school’s special‑education team to craft an Individualized Education Plan (IEP) that includes seizure‑action plans, extra time for tests, and a quiet space for breaks. Let teachers know the signs of a seizure so they can act fast.
Nutrition & Sleep
Good sleep hygiene can lower seizure thresholds. Aim for consistent bedtime routines and a cool, dark bedroom. For nutrition, if you’re on a ketogenic diet, a dietitian’s guidance is essential to avoid deficiencies.
Emotional Support
It’s normal to feel a roller‑coaster of emotions—fear, guilt, hope. Joining a support group (like the Epilepsy Foundation’s local chapter) connects you with families walking a similar path. Sharing stories can turn isolation into community.
Future Outlook
Research is moving fast. In the next few years, we expect:
- Gene‑editing trials that aim to correct faulty transport proteins directly in the brain.
- Biomarker breakthroughs—blood tests that catch metabolic imbalances before seizures start.
- AI‑driven EEG analysis that predicts seizure onset minutes in advance, giving families time to intervene.
While these advances are still on the horizon, the momentum is encouraging. The more data we gather (through registries, patient‑reported outcomes, and collaborative studies), the closer we get to turning severe epileptic encephalopathy from a “progressive threat” into a “manageable condition.”
Takeaway
Severe epileptic encephalopathy is undeniably tough, but you’re not powerless. By understanding the underlying mechanisms—like how a faulty transport protein can derail neuron metabolism—you can work with a dedicated medical team to develop a plan that protects the brain, reduces seizures, and preserves quality of life. Early diagnosis, personalized treatment, and a supportive community are your best allies.
If you or someone you love is navigating this journey, reach out to a pediatric epilepsy specialist, explore the resources linked above, and remember: every small victory—fewer seizures, a new word, a brighter smile—adds up to a brighter future.


















Leave a Reply
You must be logged in to post a comment.