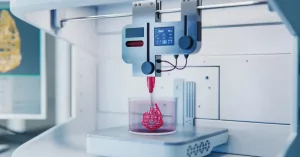
Imagine a tiny “ink” that you can squeeze out of a printer and watch it form clusters of living, insulin‑making cells—right before your eyes. That’s exactly what scientists have achieved with a new bioink for diabetes, and it could mean a world where daily insulin shots become a thing of the past.
In the next few minutes we’ll explore how this breakthrough works, why it matters for type 1 diabetes treatment, and what the road ahead looks like. Grab a coffee, settle in, and let’s dive into the future of diabetes care together.
What Is Bioink?
Definition & Core Components
At its heart, a bioink is a specially formulated hydrogel that can hold living cells while being printable. For diabetes, researchers add a cocktail of extracellular‑matrix (ECM) proteins—laminin, collagen IV, and even tiny fragments of real pancreatic tissue—to create an environment that feels “homey” to beta cells (the insulin‑producing stars of the pancreas).
How It Differs From Generic Ink
| Feature | Standard Alginate Ink | Pancreas‑Derived Bioink (e.g., PINE) |
|---|---|---|
| ECM Content | Low (mostly alginate) | High – includes laminin, collagen IV, dECM |
| Cell Viability (24 h) | ~70 % | ~90 % |
| Insulin Secretion | Minimal | Robust, glucose‑responsive |
| Immune Shielding | None | Encapsulation possible |
That extra “pancreatic” touch is what lets the ink coax stem‑derived cells into behaving like real beta cells.
Who’s Building It?
Several teams are in the game. The European ERC‑funded “Uniink” project, led by Javier Ramón Azcón, created microspheres loaded with insulin‑secreting cells that stay safe from the immune system (according to a 2023 news‑medical report). In South Korea, POSTECH’s “PINE” bioink earned a spot in Nature Communications (2025) for its ability to print functional islet‑like aggregates (a study shows). And over in the U.S., Fluicell’s Nexocyte system is already printing artificial islets on a transplantable scaffold.
How Does It Print?
The Step‑by‑Step Process
- Mix the bioink. Pancreatic dECM is blended with stem‑cell‑derived beta cells at 37 °C.
- Load the printer. A nozzle no larger than 200 µm deposits droplet after droplet onto a moving stage.
- Cross‑link. Gentle UV or ionic treatment solidifies the structure without harming the cells.
- Culture & mature. The printed construct sits in a bioreactor for 7‑14 days, allowing cells to organize and start secreting insulin.
Building the “Islet‑Like” Niche
The magic lies in recreating the tiny vascular web that nourishes real islets. POSTECH’s HICA‑V platform arranges cells around micro‑channels, letting glucose and oxygen diffuse exactly as they would in a living pancreas. The result? An islet that not only looks like the original but also reacts to glucose spikes with a brisk insulin burst.
Testing the Function
Researchers shove the printed islet into a glucose‑challenge bath. If the insulin spikes two‑ to three‑fold compared to random cell clusters, they’ve hit the sweet spot. In the PINE study, insulin output was 2.3 × higher than in suspension cultures, a clear sign of functional maturity.
Shielding From the Immune System
Even the most perfect islet would be rejected without protection. Both Uniink and Fluicell wrap their prints in a thin alginate‑PEG shell that blocks immune cells but still lets glucose and insulin pass. Think of it as a high‑tech “bubble wrap” that keeps the cells safe while they do their job.
Real‑World Impact
Why It Matters for Type 1 Diabetes
Right now, more than 4 million people in the U.S. live with type 1 diabetes, relying on multiple daily insulin injections or a pancreas transplant that’s scarce and risky. A 3D printed islet that produces insulin on demand could eliminate those injections and reduce the chance of severe complications like heart disease or kidney failure.
Ongoing Pre‑Clinical Work
In mouse models, Uniink’s encapsulated microspheres restored normal blood sugar for over three months without any immunosuppression. Fluicell’s Nexocyte implants have shown stable insulin release for 90 days in diabetic rats, and the team is now gearing up for a first‑in‑human safety trial.
First‑in‑Human Trials on the Horizon
Regulators such as the FDA and EMA are already reviewing these platforms under “Regenerative Medicine Advanced Therapy” pathways. If Phase I trials (expected late 2025) confirm safety, Phase III could follow by 2028, bringing commercial availability sometime in the early 2030s.
Related Innovations
Beyond bioink, the field is buzzing with 3D bioprinting islets that incorporate vascular cells, oxygen‑releasing particles, and even tiny glucose sensors that regulate insulin output automatically. The ecosystem is growing fast, and each breakthrough builds on the others.
Benefits & Risks – The Full Picture
Clinical Benefits
- Physiological glucose control. The printed islet senses blood sugar instantly and releases insulin proportionally, just like a native pancreas.
- No daily needles. Patients could live free from multiple injections, reducing injection‑site infections and “diabetes burnout.”
- Lower long‑term complications. Stable glycemic control slashes the risk of heart attacks, strokes, and kidney disease.
Safety & Risk Considerations
- Immune rejection. Even with encapsulation, some cells may leak antigens that trigger a response.
- Hypoglycemia risk. An over‑active implant could flood the bloodstream with insulin.
- Manufacturing consistency. Producing identical bioink batches at scale is technically demanding.
Ethical & Accessibility Issues
Personalized bioink isn’t cheap. If the technology stays confined to high‑income countries, a new health disparity could emerge. That’s why many research groups are partnering with global health NGOs to develop low‑cost production methods.
How Scientists Are Mitigating Risks
Dual‑layer encapsulation (a physical barrier plus an immunomodulatory coating) is now standard. Some teams embed real‑time glucose sensors in the implant, allowing clinicians to shut down the device remotely if insulin levels spike too high. Ongoing pre‑clinical studies also monitor long‑term tumorigenicity to ensure the cells don’t go rogue.
Future Outlook
Next‑Gen Bioinks
Researchers are spicing up the recipe with growth‑factor‑laden microspheres that coax blood‑vessel formation right inside the printed construct, improving oxygen delivery and longevity.
AI‑Driven Design
Machine‑learning algorithms now predict the optimal ECM composition for beta‑cell maturation, cutting trial‑and‑error time by half. Imagine a future where a computer tells you the perfect mix of proteins for each patient’s cells.
Smart, Integrated Implants
Picture a tiny “smart pancreas” that reads glucose levels and adjusts insulin output autonomously, all while sending data to your smartphone. That’s the direction many biotech start‑ups are headed.
Global Collaboration Networks
From the ERC‑funded Uniink consortium in Europe to POSTECH’s Korean team and Fluicell’s US lab, the field thrives on cross‑border cooperation. Shared data repositories and open‑source bioink recipes accelerate progress for everyone.
Timeline for Patients
- 2025‑2026: First safety‑only human trials.
- 2028‑2030: Pivotal Phase III efficacy studies.
- Early 2030s: Commercial launch (estimated).
While we’re not there yet, the pace feels like a sprint rather than a crawl. The excitement in conference halls (remember the buzz at ESOT 2025?) tells us that the community believes this is more than a pipe‑dream.
Conclusion
We’ve traveled from the humble concept of a printable “ink” to a future where a tiny, 3‑D‑printed organ patch could replace a lifelong regimen of insulin shots. The science of bioink for diabetes is proving that we can coax stem cells into forming functional human islets, protect them from the immune system, and deliver them safely into patients. Projects like Uniink, POSTECH’s PINE platform, and Fluicell’s Nexocyte showcase how quickly these ideas move from the lab bench to the bedside.
If you’re curious about the broader landscape, check out more on functional human islets or learn how 3D printed islets are shaping the next generation of type 1 diabetes treatment. The journey is just beginning, and each discovery brings us a step closer to a world where diabetes is no longer a daily burden.
What do you think about this emerging technology? Could a bio‑ink‑based islet be the answer you’ve been hoping for, or do you see challenges we haven’t considered yet? Feel free to share your thoughts—together, we’ll keep the conversation alive and push the science forward.























Leave a Reply
You must be logged in to post a comment.