Got a diagnosis that feels like a ticking time bomb? When diabetes hits a severe stage—think diabetic ketoacidosis (DKA), hyperosmolar hyperglycaemic state (HHS), or a constantly rising A1C—right‑now answers matter more than historical background. Below you’ll find the quickest ways to stay alive, the medicines that keep you steady, and the hopeful, cutting‑edge options that might one day change the game. All of it in a friendly, down‑to‑earth chat you can actually read without a PhD.
Emergency Care Essentials
What Are DKA and HHS?
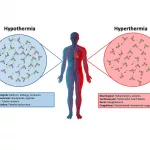
DKA and HHS are the two life‑threatening emergencies that most people associate with “severe diabetes.” DKA usually shows up in Type 1 patients when insulin stops working, causing a dangerous buildup of ketones and a blood‑sugar spike above 250 mg/dL. HHS, on the other hand, tends to affect Type 2 folks and pushes glucose levels even higher—often over 600 mg/dL—without major ketone production.
Both conditions share common red‑flags: extreme thirst, rapid breathing, confusion, and, if left untreated, loss of consciousness. Think of them as the body’s SOS signal saying, “I’m out of fuel and need help now!”
First‑Line Hospital Management
| Step | What’s Done | Why It Matters |
|---|---|---|
| IV Fluids | Large‑volume saline (sometimes with electrolytes) | Replaces lost water, corrects dehydration, and improves blood pressure. |
| Insulin Infusion | Continuous short‑acting insulin drip | Stops ketone production and pulls glucose into cells. |
| Electrolyte Replacement | Potassium, magnesium, and phosphate as needed | Prevents dangerous heart‑rhythm problems. |
| Treat Underlying Trigger | Antibiotics for infection, fluids for dehydration, etc. | Stops the chain reaction that started the crisis. |
According to Milton Keynes University Hospital, aggressive fluid resuscitation and insulin are the cornerstones of treatment, while electrolyte monitoring prevents the hidden, silent dangers of cardiac arrest.
After‑Care: Keeping the Storm at Bay
Surviving the emergency is just the first chapter. The real work starts when you’re back home and need to avoid a repeat episode. Here’s a quick checklist:
- Carry a glucagon kit and know how to use it.
- Set a “sick‑day” rule: double‑check blood sugar every 2‑3 hours if you’re ill.
- Stay hydrated—water helps kidneys flush excess glucose.
- Schedule a follow‑up with your endocrinologist within a week.
If you’re curious about how a diabetes cure might look down the road, keep reading. The road to remission starts with solid everyday habits.
Core Medication Options
Insulin – The Backbone for Severe Cases
When glucose is through the roof, insulin is the rescue squad. You’ll encounter three major families:
- Rapid‑acting (lispro, aspart) – taken right before meals to catch the post‑meal surge.
- Short‑acting (regular) – works slightly slower; often used in hospitals.
- Long‑acting (glargine, detemir) – provides a steady basal level.
The benefits are obvious: rapid glucose control and flexibility. The downsides? Hypoglycemia, weight gain, and the need for frequent blood‑glucose checks. That’s why many patients ask, “Can I ever get off insulin?” The answer is nuanced; most severe cases will need a basal dose for life, but adjunct therapies can dramatically reduce the amount you need.
Non‑Insulin Medications That Complement Insulin
| Class | Example | When It’s Added | Key Pros / Cons |
|---|---|---|---|
| GLP‑1 Receptor Agonists | Semaglutide | High BMI, cardiovascular risk | Weight loss, low hypoglycemia risk / GI side‑effects |
| SGLT2 Inhibitors | Empagliflozin | Kidney disease, heart‑failure | Heart‑protective, can cause ketoacidosis / urinary infections |
| DPP‑4 Inhibitors | Sitagliptin | Modest A1C reduction needed | Mild side‑effects, modest efficacy |
A 2024 American Diabetes Association guideline notes that combining a basal insulin with a GLP‑1 agonist often yields the best A1C drop while limiting weight gain. That’s the sweet spot for many people living with severe diabetes.
Managing Side‑Effects & Ongoing Monitoring
Even the best regimen can feel like a juggling act. Here’s a quick monitoring cheat‑sheet:
- Check fasting glucose at least twice weekly.
- Record A1C every 3 months.
- Annual kidney (eGFR) and eye exams.
- Discuss any persistent hypoglycemia with your doctor – it may signal the need to lower the insulin dose.
If you’re craving a future without daily shots, keep an eye on the insulin‑free treatment research that’s blossoming in academic centres. It’s not a miracle, but a genuine avenue for dose reduction.
Cutting‑Edge Emerging Therapies
Stem‑Cell‑Based Approaches
Stem cells are the sci‑fi buzzword that’s slowly creeping into real‑world clinics. In a typical stem cell trial, researchers inject mesenchymal stem cells (MSCs) into the bloodstream, hoping they’ll home to the pancreas and revive dying beta‑cells.
Early‑phase data show modest improvements in fasting glucose and, in a handful of participants, a reduced insulin requirement. But remember, most trials are Phase 1 or 2, meaning safety is still being hammered out, and long‑term durability is unknown.
How to Find a Legitimate Trial
- Visit ClinicalTrials.gov and filter for “type 1 diabetes” or “type 2 diabetes” plus “stem cell”.
- Ask your endocrinologist to verify the sponsor’s credentials.
- Avoid clinics that demand full payment up‑front; reputable trials cover costs.
Regenerative Programs and FDA‑Approved Cell Products
Some companies, like the ones behind stem cell therapy diabetes, market “insulin‑resensitizing” protocols. The U.S. Food and Drug Administration has cleared a few cell‑based products (e.g., A1C Therapy’s Physiologic Insulin Resensitization), but the evidence is still emerging. A study from the Schull Institute (2015) reported a 63 % reduction in reported HbA1c among 60 participants—but note the retrospective design; larger, blinded trials are needed.
Gene‑Editing and Islet‑Cell Encapsulation
CRISPR‑based editing of the insulin gene and encapsulated islet transplants are fascinating, yet they belong to the “future‑tech” shelf for now. If you’re reading this in 2025, keep an eye on ongoing Phase 1 data, but don’t gamble your health on unproven claims.
Practical Lifestyle Strategies
Nutrition‑First Tactics for Severe Diabetes
Food can be a powerful medicine—if you give it the right script. Low‑carb or ketogenic eating has been shown to reduce insulin requirements dramatically. A 2024 review in Diabetes Care concluded that a carbohydrate intake below 50 g per day lowered the average basal insulin dose by 30 % in patients with long‑standing Type 2 diabetes.
Here’s a simple starter plan:
- Breakfast: 2 eggs, spinach, and avocado (≈ 5 g carbs).
- Lunch: Grilled chicken salad with olive‑oil dressing (≈ 10 g carbs).
- Dinner: Salmon, roasted broccoli, and a small side of quinoa (≈ 15 g carbs).
- Snacks: Handful of nuts or a piece of cheese.
Hydration matters too—water helps kidneys clear excess glucose, and limiting sugary drinks removes a major source of spikes.
Safe Exercise for High‑Risk Patients
Movement is medicine, but severe diabetes demands a gentle approach. Aim for 150 minutes of moderate cardio per week—think brisk walks, stationary cycling, or water aerobics. Add two sessions of resistance training (light dumbbells or body‑weight squats) to improve insulin sensitivity.
Watch for warning signs: dizziness, rapid heart rate, or a sudden drop in blood glucose. If you feel any of these, stop, snack on a quick carbohydrate, and re‑check your level.
Weight‑Loss Interventions: When Size Matters
Even a modest 5 % weight loss can shave off medications and improve A1C. For those with a BMI > 35 kg/m², bariatric surgery has become a recognized “metabolic” procedure—studies show up to 80 % of patients achieve remission within two years.
Real‑World Success Stories (Experience)
Take Maya, a 52‑year‑old with a 12‑year history of Type 2 diabetes. After a DKA admission, she joined a multidisciplinary program that combined low‑carb nutrition, GLP‑1 therapy, and a 6‑month supervised exercise plan. Within nine months, her A1C dropped from 9.8 % to 6.4 %, and she reduced her basal insulin from 30 U to 5 U per day. Stories like Maya’s illustrate that “severe” does not equal “hopeless.”
Personal Treatment Decision
Decision‑Making Framework
Choosing the right therapy feels like picking a movie on Netflix—there are many options, each with its own rating, genre, and runtime. Use this simple matrix:
| Option | Efficacy (A1C drop) | Side‑Effect Profile | Cost & Insurance | Lifestyle Fit |
|---|---|---|---|---|
| Basal‑Bolus Insulin | 1.5‑2 % | Hypoglycemia, weight gain | Covered, low out‑of‑pocket | Requires daily injections & monitoring |
| GLP‑1 + Low‑dose Insulin | 2‑3 % | GI upset, rare pancreatitis | Partial coverage, moderate co‑pay | Weekly injection, less monitoring |
| Stem‑Cell Trial | Variable (early data ~1 %) | Unknown long‑term safety | Usually free (research‑funded) | Requires travel to trial site |
| Low‑Carb + Lifestyle | 1‑2 % (if adhered) | Minimal | Very low | High self‑discipline needed |
Put a score on each column (1‑5) and add them up. The highest total often points to the most balanced choice for you.
When to Seek a Second Opinion
Any time you encounter:
- “Miracle cure” promises with no peer‑reviewed data.
- Up‑front payment demands for “experimental” therapies.
- Vague safety information or missing clinical trial IDs.
Trustworthy clinicians will welcome a second look and give you a clear explanation of risks versus benefits.
Final Takeaway Summary
Severe diabetes is a serious, sometimes frightening, diagnosis—but it isn’t a life sentence. Immediate emergency care—IV fluids, insulin infusion, and electrolyte management—keeps you alive. Long‑term, a mix of basal insulin, smart adjunct medicines, and disciplined lifestyle changes can bring glucose under control and reduce complications.
On the horizon, stem‑cell trials, regenerative cell products, and gene‑editing research whisper of a future where “insulin‑free” might be more than a tagline. Until then, the best strategy is a balanced one: know the warning signs, stay on top of monitoring, and partner with a knowledgeable medical team.
If you feel overwhelmed, remember you’re not alone. Reach out to your healthcare provider, explore reputable clinical trials, and consider joining a support community. Your journey may be tough, but with the right tools and a dose of optimism, you can steer it toward a healthier tomorrow.






















Leave a Reply
You must be logged in to post a comment.