In a world where chronic diseases feel like relentless shadows, a stem cell trial can feel like the ray of sunrise some of us have been waiting for. Short‑answer? A stem cell trial is a carefully‑designed clinical study that tests whether stem‑cell‑based therapies are safe and effective for humans. For people battling severe diabetes, it’s a possible gateway to an insulin‑free treatment or even a true diabetes cure. Below, I walk you through what these trials look like, why they matter, and how you can decide if one is right for you.
What Is a Stem Cell Trial
Definition & Phases
Think of a clinical study as a road trip with checkpoints. Phase I checks the map (safety), Phase II looks at the scenery (early efficacy), and Phase III tests the route at scale (large‑scale effectiveness). A stem cell trial follows the same steps, but the “vehicle” is a living cell that can turn into many different cell types.
Types of Stem Cells Used
There are several families of stem cells you might hear about:
- Embryonic stem cells – pluripotent, can become any cell type, but raise ethical concerns.
- Adult (somatic) stem cells – harvested from bone marrow, fat, or blood; often used for “autologous” (your own) therapies.
- Mesenchymal stem cells (MSCs) – a versatile adult type known for calming inflammation.
- Induced pluripotent stem cells (iPSCs) – adult cells re‑programmed back to a pluripotent state.
Trial Design Basics
Most rigorous trials are randomized, double‑blind, placebo‑controlled. That means participants are randomly assigned to receive either the stem‑cell product or a sham injection, and neither the patient nor the doctor knows which they got until the study ends. This design keeps bias at bay, letting the data speak for itself.
Regulatory Oversight
In the United States, the FDA and Institutional Review Boards (IRBs) review every protocol. Similar agencies exist in Europe (EMA) and elsewhere, ensuring safety standards are met before the first patient steps into the clinic.
Why Stem Cell Trials Matter for Diabetes
Limits of Current Insulin Therapy
Living with Type 1 or advanced Type 2 diabetes often feels like you’re tethered to a pump or a dozen daily injections. Even with the newest analog insulins, many patients battle unpredictable highs and lows, and the constant vigilance can wear anyone down. That’s why researchers are hunting for a solution that restores the body’s own ability to make insulin.
Regenerating β‑Cells
Stem cells have the unique ability to differentiate into pancreatic β‑cells—the very cells that produce insulin. Early animal studies showed that transplanted stem‑derived β‑cells can sense glucose levels and release insulin just like native cells. If this works in people, it could usher in an insulin‑free treatment and dramatically improve quality of life.
Real‑World Stories
Take Maya, a 42‑year‑old marketing director who’s lived with Type 1 diabetes for 20 years. After joining a Phase I trial at a major academic center, she says the weekly glucose spikes that used to dictate her schedule have smoothed out. “I still need insulin,” she tells me, “but the doses are lower and my mood is steadier. It feels like a safety net that’s finally in place.” Stories like Maya’s highlight both the hope and the early‑stage nature of the research.
Related Treatments to Watch
For a deeper dive into how stem‑cell research dovetails with other innovative approaches, check out our guide on stem cell therapy diabetes. It walks through the science while keeping the jargon at bay.
Top Current Stem‑Cell Trials
Neural Stem Cells for Chronic Stroke (Stanford)
One of the most rigorously monitored studies is a Phase 1/2A trial (NCT04631406) that injects modified stromal cells (SB623) directly into the brains of patients who suffered an ischemic stroke more than six months ago. According to the trial’s public record, the therapy was safe and showed early hints of motor improvement (source).
Mesenchymal Cells for Bipolar Disorder (UTHealth Houston)
Although not diabetes‑focused, this double‑blind, placebo‑controlled trial uses allogeneic MSCs to calm brain inflammation. Participants report better energy and mood, underscoring the anti‑inflammatory power of stem cells—a mechanism also relevant to protecting pancreatic islets (source).
SCOTS – Stem Cell Ophthalmology Treatment Study
The SCOTS program, led by researchers like Dr. Jeffrey Weiss, has treated retinal and optic‑nerve diseases with bone‑marrow‑derived stem cells. Early data show that 61 % of treated eyes improved, while only 14 % worsened (study). The eye is an excellent “test bed” for stem‑cell delivery because it’s easy to image and monitor.
COVID‑19 ARDS Trial (Stemedica)
In a Phase II study, intravenously delivered MSCs lowered oxygen requirements within 48 hours for patients with severe ARDS. The investigators attribute this to the cells’ secretion of growth factors and anti‑inflammatory cytokines (press release).
Comparison Table
| Trial | Phase | Disease Target | Cell Type | Delivery | Status |
|---|---|---|---|---|---|
| Stanford Stroke | 1/2A | Chronic Ischemic Stroke | Modified Stromal (SB623) | Intracerebral Injection | Recruiting |
| UTHealth Bipolar | II | Treatment‑Resistant Bipolar | Allogeneic MSCs | Intravenous | Active |
| SCOTS Ophthalmology | I/II | Retinal/Optic Nerve Disease | Bone‑Marrow MSCs | Retro‑bulbar Injection | Ongoing |
| Stemedica COVID‑19 | II | Severe ARDS | Ischemic‑Tolerant MSCs | IV Infusion | Completed Enrollment |
Benefits & Risks of Joining
Potential Benefits
- Regeneration: Stem cells may replace damaged tissue (e.g., β‑cells).
- Anti‑Inflammatory Effects: MSCs often dampen harmful immune responses.
- Access to Cutting‑Edge Care: Participants receive close monitoring by top specialists.
- Hope for an diabetes cure: While not guaranteed, many view trials as the most promising path forward.
Safety Considerations
Every medical intervention carries risk. In stem‑cell trials, the most commonly reported side effects are mild: soreness at the injection site, temporary fever, or short‑lived flu‑like symptoms. Rare but serious concerns include:
- Immune rejection (especially with allogeneic cells).
- Uncontrolled growth leading to tumor formation—something regulators watch closely.
- Infection from the procedure itself.
According to a 2023 FDA safety briefing, serious adverse events in early‑phase stem‑cell studies occur in less than 2 % of participants (FDA brief).
Financial & Logistical Factors
Most trials cover the investigational product and core medical costs, but you may still pay for travel, lodging, or ancillary tests. Insurance rarely reimburses experimental therapies, though some programs offer stipends. It’s wise to ask the trial coordinator up front about any out‑of‑pocket expenses.
Evaluating Credibility
Before signing up, run through this quick checklist:
- Is the study listed on ClinicalTrials.gov with a clear ID?
- Has an Institutional Review Board (IRB) approved it?
- Are the investigators affiliated with reputable institutions (e.g., university medical centers)?
- Do peer‑reviewed publications accompany the trial (Nature, Cell Stem Cell, etc.)?
- Is there transparent information about risks, benefits, and withdrawal procedures?
How to Find a Legitimate Trial
Search ClinicalTrials.gov
Start with the keyword “stem cell trial” and filter by “Recruiting” and the disease you care about (e.g., “diabetes”). The site shows the trial’s phase, sponsor, and contact details.
Ask Your Doctor
Endocrinologists and diabetes specialists often have connections to academic centers. A quick conversation can reveal whether a trial matches your health profile.
Verify IRB Approval
Every legit trial will have an IRB reference number. If it’s missing, walk away.
Read Patient Forums (With Caution)
Websites like Diabetes Daily or Reddit’s r/diabetes can provide personal anecdotes, but cross‑check any claims with scientific sources.
Sample Email to a Coordinator
“Hello Dr. Smith, I’m a 38‑year‑old with Type 1 diabetes and I’m interested in learning more about the stem‑cell trial (NCT XXXXX). Could you share eligibility criteria and the time commitment required? Thank you.”
Future Outlook: When Might Stem‑Cell Therapy Become Main‑Line?
Pipeline Timeline
Most experts predict that, if Phase III data remain positive, a regulated stem‑cell product for diabetes could seek FDA approval within the next 5–7 years. That timeline mirrors the journey of other biologics such as CAR‑T cells, which moved from early trials to market in roughly six years.
Regulatory Hurdles
Regulators require convincing evidence that the therapy is safe and consistently produces the desired cell type. Manufacturing also needs to be scalable—meaning a single donor line must reliably generate billions of cells under Good Manufacturing Practice (GMP) conditions.
Emerging Technologies
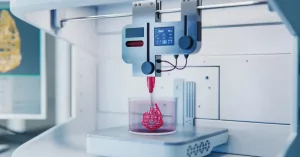
Gene‑edited stem cells (CRISPR‑modified) aim to protect transplanted β‑cells from autoimmune attack. 3‑D bioprinting is already being used to create scaffold‑supported “mini‑islets” that can be implanted under the skin. These advances could eventually turn a severe diabetes treatment into something as routine as a flu shot.
Conclusion
Navigating a stem cell trial is not a decision to take lightly, but it can also be a courageous step toward a future where diabetes no longer dictates every meal and every mood. By understanding the trial phases, weighing the benefits against the risks, and verifying the credibility of each study, you empower yourself with the knowledge that many patients lack.
If you’re curious about whether a trial could be a fit for you—or if you simply want to stay updated on the latest breakthroughs—start by browsing ClinicalTrials.gov, talk to your healthcare provider, and keep an eye on reputable news from academic centers. Remember, the science is moving fast, and your participation could help shape the next generation of therapies for you and countless others.
Feel free to explore more on our site: stem cell therapy diabetes, severe diabetes treatment, insulin‑free treatment, and diabetes cure. Your journey might just inspire someone else to take the first step, too.





















Leave a Reply
You must be logged in to post a comment.