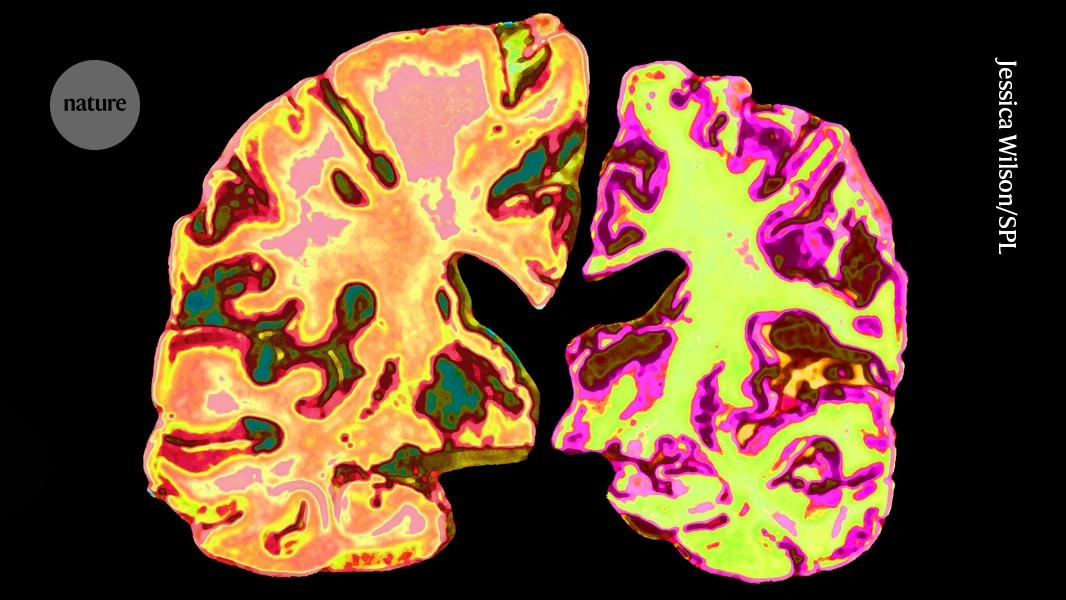
Looking for ways to slow or even reverse Alzheimer’s without relying on the usual prescription pills? You’re not alone. Many families are asking the same question, and the good news is that a growing body of research points to several evidence‑based alternatives that can make a real difference. In this article we’ll walk through the most promising options— from movement and nutrition to low‑dose “exercise‑mimic” drugs— so you can decide what feels right for you or your loved one.
Why Look Beyond Drugs
Traditional Alzheimer’s medicines can help with symptoms, but they often come with modest benefits, side‑effects, and high costs. Even the newest disease‑modifying antibodies have shown mixed results in large trials. That’s why many clinicians and caregivers are exploring a balanced approach: keep the proven drugs if they work, but also layer on lifestyle and emerging therapies that target the disease from different angles.
Balancing benefits and risks is essential. For example, a low‑dose lithium supplement may show memory‑boosting effects in mice, yet it requires careful blood‑level monitoring to avoid toxicity. Likewise, regular exercise carries almost no medical risk and offers a host of cardiovascular and emotional perks. The key is to combine what’s safe, what’s supported by data, and what fits into everyday life.
Lifestyle‑Based Alternatives
When we talk about “alternatives,” we usually start with the basics: movement, food, sleep, and mental engagement. These pillars work together to create a brain‑friendly environment that can slow cognitive decline and improve quality of life.
Exercise: Brain’s Natural Drug
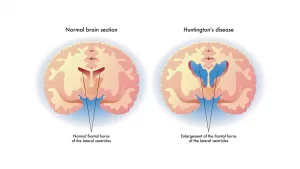
If you’ve ever felt that “runner’s high,” you’ve tasted a glimpse of what exercise can do for the brain. Physical activity spikes the production of brain‑derived neurotrophic factor (BDNF), a protein that fuels new neuron growth and strengthens connections in the hippocampus—the memory center most vulnerable to Alzheimer’s.
Research shows that just 150 minutes of moderate aerobic activity each week can produce cognitive gains comparable to some prescription drugs. A recent mouse study even found that low‑dose lithium mimics many of these exercise‑induced changes, suggesting that the two strategies may reinforce each other.
Want to see the science behind the “cognitive benefits of exercise”? Check out this article on the cognitive benefits of exercise. It breaks down the mechanisms in plain language and gives you a quick‑start checklist.
Sample Weekly Workout
| Day | Activity | Duration |
|---|---|---|
| Monday | Brisk walk or stationary bike | 30 min |
| Tuesday | Resistance band training (upper & lower body) | 20 min |
| Wednesday | Walking + light jogging intervals | 30 min |
| Thursday | Yoga or balance drills | 25 min |
| Friday | Swimming or water aerobics | 30 min |
| Saturday | Family dance party (fun cardio) | 30 min |
| Sunday | Rest & gentle stretching | — |
Notice how the plan blends cardio, strength, and flexibility—exactly the mix that research says supports memory. And if you’re wondering whether a “workout for dementia” looks different, the answer is no; the same principles apply, only the intensity may be adjusted. See a practical guide here for a workout for dementia.
Nutrition and Supplements
What we put on our plates can either feed the brain or fuel inflammation. Below is a snapshot of the most studied nutrients that have shown promise in slowing Alzheimer’s progression.
| Strategy | Evidence (Year) | Key Takeaway |
|---|---|---|
| Low‑dose Lithium | 2025 mouse model (UCLA) | Reverses memory loss; needs medical supervision |
| Omega‑3 DHA | 2024 meta‑analysis | Boosts synaptic health, modest cognitive gain |
| Curcumin + Piperine | 2023 pilot trial | Reduces neuro‑inflammation, improves mood |
| B‑vitamin complex | 2022 RCT | Lowers homocysteine, modest memory benefit |
One easy way to incorporate these nutrients is to aim for a Mediterranean‑style diet: fatty fish (salmon, sardines) twice a week, a rainbow of vegetables, extra‑virgin olive oil, and a handful of nuts daily. If you’re curious about how a “low‑dose lithium” regimen looks in practice, talk to a neurologist—this isn’t something to self‑prescribe.
For those seeking a more pharmaceutical‑like approach, there’s a whole category of emerging “exercise‑mimic” drugs. These compounds aim to trigger the same molecular pathways that get activated during physical activity, like AMPK and PGC‑1α, without the need to lace up shoes every day.
Emerging Mimic Drugs
So what exactly is an “exercise‑mimic” drug? In simple terms, it’s a molecule that tricks the body into thinking it’s just completed a workout, leading to the release of brain‑friendly chemicals. Scientists are especially excited about a handful of candidates that have already entered early‑phase human trials.
Current Candidates
| Drug / Compound | Mechanism | Status |
|---|---|---|
| Enbrel® (Etanercept) | Blocks TNF‑α, reducing inflammation | Small pilot for Alzheimer’s, 2024 |
| Metformin (low dose) | Activates AMPK, improves insulin signaling | Phase II trial ongoing |
| Resveratrol analogs | SIRT1 activation, mimics caloric restriction | Pre‑clinical mouse data |
| Low‑dose Lithium | Inhibits GSK‑3β, protects neurons | Mouse → early human safety |
If you want a deeper dive into these “exercise mimic drugs,” this exercise mimic drugs guide explains how each works, what the current research says, and when you might consider them under a doctor’s supervision.
Safety Checklist
- Get baseline blood work (kidney, thyroid, electrolytes).
- Monitor serum lithium levels if you try low‑dose lithium.
- Discuss any existing meds—some compounds interact with blood thinners or diabetes drugs.
- Start with the lowest effective dose and adjust only under medical guidance.
Remember, these are still experimental. A study in Nature Communications highlighted a protein drug that suppressed early amyloid‑driven hyperactivity in mice, but the researchers stress that human trials are still years away.
Non‑Pharmacological Therapies
Beyond movement and nutrients, other “soft” therapies can enrich brain health. Mind‑body practices like meditation, tai chi, or even simple deep‑breathing exercises lower cortisol, a hormone that, when chronically high, can accelerate amyloid formation.
Neuro‑feedback and gentle brain‑stimulation devices have also entered the market with FDA clearance for safety. Though the evidence is still emerging, many users report improved focus and mood after short‑term sessions.
Stem‑cell research is another frontier. A 2023 study from UC‑San Diego showed that transplanting hematopoietic stem cells reduced neuroinflammation and plaque buildup in mice. While exciting, these approaches remain experimental and are typically only available in research settings.
Build a Personal Plan
So, how do you turn all this information into a concrete action plan? Here’s a simple, step‑by‑step framework that you can adapt to any lifestyle.
Step 1 – Medical Baseline
Schedule a full neurologic workup: cognitive testing (MoCA or MMSE), blood panels (vitamin D, B‑12, thyroid), and a brain scan if recommended. Knowing where you start helps you measure progress later.
Step 2 – Lifestyle Audit
Write down a typical day: meals, activity, sleep hours, stress triggers. Identify one or two areas where you can make immediate, realistic changes.
Step 3 – Pick 2–3 Evidence‑Based Alternatives
- Start a structured walking program (see the weekly table above).
- Add a Mediterranean‑style dinner twice a week.
- Discuss low‑dose lithium or metformin with your physician if you’re comfortable with medication.
Step 4 – Set Measurable Goals
Examples: “Walk 30 minutes, five days a week for three months,” or “Increase MoCA score by 2 points in six months.” Small, trackable goals keep motivation high.
Step 5 – Monitor & Adjust
Every 12 weeks, re‑run the cognitive test, review blood work, and note any side effects. If something isn’t working, tweak it—maybe swap resistance training for a swimming session, or adjust supplement dosage.
For a printable version of this roadmap, consider creating a simple spreadsheet with columns for “Done,” “In‑Progress,” and “Planned.” Seeing your progress on paper can be incredibly rewarding.
Bottom Line
Alzheimer’s treatment alternatives span a spectrum—from everyday habits like walking and eating fish to cutting‑edge low‑dose drugs that mimic the chemistry of exercise. Each option brings its own set of benefits and risks, which is why a personalized, balanced plan—crafted with a trusted healthcare professional—is the smartest way forward.
Remember, you’re not alone on this journey. Whether you start with a 10‑minute walk after dinner or explore a conversation about low‑dose lithium with your doctor, every positive step adds up. If you’ve tried any of these strategies, or if you have questions about tailoring them to your situation, feel free to reach out. Together we can turn hope into action.


















Leave a Reply
You must be logged in to post a comment.