If you’ve ever felt the weight of a dark cloud that just won’t lift, you know how tempting the idea of a quick fix can be. The good news? Antidepressants really can help lift that cloud—but the right one for you depends on a lot of personal details, from your symptoms to your lifestyle. Below is a friendly, down‑to‑earth guide that walks you through how these medications work, the different families they belong to, special situations you might face, and how to stay safe while you’re on them. Think of it as a coffee‑shop chat with a friend who’s done a lot of reading, talked to doctors, and listened to real stories.
Why Meds Help
How antidepressants target brain chemistry
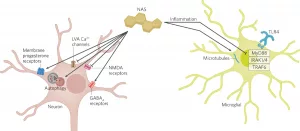
Depression isn’t just “being sad”—it’s a mess of chemicals in the brain that get out of sync. Most antidepressants aim to restore balance among neurotransmitters like serotonin, norepinephrine, dopamine, and even the GABA system. Think of these messengers as traffic lights; when one stays red for too long, traffic jams (low mood, fatigue, anxiety) happen. Antidepressants either turn more lights green (more serotonin) or keep the reds from staying on too long.
When medication is recommended
Doctors usually consider pills when depression is moderate to severe, when it’s been lasting more than a few weeks, or when symptoms don’t improve with therapy alone. If you’ve tried talk therapy and still feel stuck, medication can give your brain that extra nudge it needs.
What “doing the right thing” looks like
The best approach is a partnership with your prescriber. Bring a list of your current meds, any past antidepressant experiences, and honest answers about side‑effects you fear. A clinician’s expertise blends with your lived experience to pinpoint the most promising option.
Quick fact box
| Statistic | What it means |
|---|---|
| 8.3% of U.S. adults | Reported a major depressive episode in 2021 (National Institute of Mental Health) |
| 61% of those adults | Received some form of treatment, often medication |
Drug Classes
SSRIs – the go‑to starter
Selective serotonin reuptake inhibitors (SSRIs) are the most common first‑line choice because they’re generally effective and have a milder side‑effect profile. Names you’ve probably heard: sertraline (Zoloft), fluoxetine (Prozac), citalopram (Celexa), escitalopram (Lexapro), and paroxetine (Paxil). They work by blocking serotonin reabsorption, leaving more of it to float around in the brain.
SNRIs – serotonin plus norepinephrine
If you struggle with both low mood and chronic pain or fatigue, a serotonin‑norepinephrine reuptake inhibitor (SNRI) may be a better fit. Duloxetine (Cymbalta) and venlafaxine (Effexor) target two neurotransmitters at once, often easing both emotional and physical symptoms.
TCAs & MAOIs – older, but still useful
Tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) belong to the “grandparent” generation of mood‑lifters. They can be powerful, especially when newer meds haven’t helped, but they also carry more dietary restrictions and side‑effects like dry mouth, constipation, or blood‑pressure spikes. A specialist usually handles them.
Atypical & newer agents – beyond the basics
These include bupropion (Wellbutrin), which nudges dopamine and norepinephrine, and drugs that act on the neurosteroid drugs pathway. Neurosteroids are a hot research area; they can act rapidly (sometimes within days) and are already approved for postpartum depression.
Choosing the right class for you
Age, other health conditions, personal history, and even how you metabolize meds matter. For example, older adults often start with lower doses to avoid dizziness, while younger patients might prioritize medications with fewer sexual side‑effects.
Comparison table
| Class | Mechanism | Typical Uses | Pros | Cons |
|---|---|---|---|---|
| SSRIs | Block serotonin reuptake | Major depression, anxiety | Well‑tolerated, once‑daily | Sexual dysfunction, GI upset |
| SNRIs | Block serotonin & norepinephrine reuptake | Depression with pain, fibromyalgia | Addresses both mood & pain | Higher blood pressure, insomnia |
| TCAs | Block reuptake of several neurotransmitters | Depression, chronic pain, migraines | Strong efficacy | Anticholinergic side‑effects, overdose risk |
| MAOIs | Inhibit monoamine oxidase enzyme | Atypical depression, PTSD | Effective when others fail | Dietary restrictions, drug interactions |
| Atypical (bupropion, neurosteroids) | Varies – dopamine boost, GABA modulation | Depression, smoking cessation, postpartum | Less sexual side‑effects, rapid action | Seizure risk (bupropion), limited long‑term data |
Special Situations
Post‑natal & postpartum depression
New mothers often face a unique hormonal roller‑coaster. While therapy is essential, medication can provide quick relief, especially if breastfeeding. Certain SSRIs (like sertraline) are considered safer for nursing infants, but the newest postpartum depression remedies include neurosteroid options such as brexanolone, which works within days.
GABA‑targeting antidepressants
Some emerging drugs modulate the GABA system, the brain’s primary inhibitory neurotransmitter. By enhancing GABA activity, they can calm the “over‑drive” often seen in anxiety‑heavy depression. Research highlighted by a recent Healthline article suggests these agents may become first‑line for mixed anxiety‑depression presentations.
Neurosteroid drugs – rapid‑acting hope
Traditional antidepressants can take weeks to show effects. Neurosteroid drugs, originally designed for seizures, have shown promise in knocking down depressive symptoms in as little as 24–48 hours. They’re already FDA‑approved for postpartum depression under the brand name brexanolone, and trials are expanding to broader adult depression.
When medication isn’t enough
Even the best pill can’t replace a supportive environment. Cognitive‑behavioral therapy (CBT), regular exercise, and sleep hygiene often boost medication benefits. If you’ve tried several meds without relief, discuss “treatment‑resistant depression” options with your doctor—alternatives like ketamine infusions or transcranial magnetic stimulation (TMS) may be viable.
Benefits vs. Risks
Common benefits
When the right drug clicks, you’ll notice:
- Improved mood and motivation
- Better sleep and appetite regulation
- Increased ability to engage in daily activities
- Reduced thoughts of self‑harm
Typical side‑effects
Most people experience at least one mild side‑effect. The most frequently reported are nausea, headache, sleep disturbances, and temporary sexual changes. Most fade within a few weeks as your body adjusts.
Serious cautions
Rare but important warnings include:
- Serotonin syndrome – a potentially life‑threatening condition if multiple serotonergic agents are combined. Symptoms: confusion, rapid heart rate, high blood pressure.
- Increased suicidality – especially in people under 25. Close monitoring during the first few weeks is crucial.
- Drug interactions – MAOIs, for instance, require you to avoid tyramine‑rich foods (cheese, cured meats) and certain over‑the‑counter meds.
Monitoring & follow‑up
Typical schedule: a check‑in at 2 weeks to gauge early response and side‑effects, another at 6 weeks to assess efficacy, and then regular 3‑month reviews. Keep a symptom journal – it makes the conversation with your clinician far smoother.
Practical Guidance
Preparing for your first appointment
Write down:
- All prescription, over‑the‑counter, and herbal products you take
- Your complete symptom checklist (sleep, appetite, mood, energy)
- Any past medication experiences – even if they were “bad”
Ask your doctor about:
- Which drug class fits your profile best?
- Possible side‑effects and how to manage them
- When to schedule follow‑up labs (e.g., liver function for certain meds)
Starting a new antidepressant
Most doctors begin with a low dose and slowly titrate up. If you miss a dose, take it as soon as you remember unless it’s almost time for the next one – then just skip the missed pill. Never double up.
When to consider switching
Give a new medication at least 4–6 weeks before deciding it’s not working. Red flags that merit an earlier change include:
- Worsening mood or emergent suicidal thoughts
- Intolerable side‑effects that persist beyond the first two weeks
- Physical symptoms like severe dizziness or rapid heart rate
Mike, a friend of mine, switched from sertraline to duloxetine after three months because his lingering nerve pain never improved. The switch gave him both mood lift and pain relief.
Lifestyle adjuncts
Medication shines when paired with healthy habits:
- Sleep: Aim for 7–9 hours; keep a regular bedtime routine.
- Movement: Even a 15‑minute walk boosts serotonin.
- Nutrition: Omega‑3‑rich foods (salmon, walnuts) may enhance response.
- Mindfulness: Simple breathing exercises can reduce anxiety that sometimes spikes when beginning a new drug.
Trusted resources
For deeper dives, the National Institute of Mental Health (NIMH) offers up‑to‑date guides, and the FDA releases safety alerts when needed. According to a recent Healthline summary, staying informed is half the battle.
Conclusion
Antidepressants are a powerful tool in the fight against depression, but they’re not a “one‑size‑fits‑all” solution. By understanding how each drug class works, weighing benefits against risks, and staying engaged with your healthcare team, you can find a medication that truly fits your life. Remember, the journey often involves trial and error, but every step brings you closer to brighter days.
Take what resonates, discuss it with a trusted clinician, and don’t hesitate to explore related topics like postnatal depression treatment or postpartum depression remedies if they apply to you. You deserve a treatment plan that honors both your mind and your unique story.





















Leave a Reply
You must be logged in to post a comment.