Quick Answer
If you’re wondering what actually helps with postpartum depression, the short answer is: a mix of evidence‑based medical treatments and safe, supportive lifestyle habits. Proven options include prescription antidepressants (especially SSRIs), FDA‑approved neurosteroid drugs that target the GABA system, omega‑3 supplements, gentle exercise, and strong social support. The right combination depends on how severe your symptoms are, whether you’re breastfeeding, and what feels doable in your daily routine.
What Is PPD
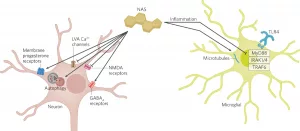
Postpartum depression (PPD) isn’t just “the baby blues.” It’s a medical condition that affects roughly 1 in 7 new mothers and can linger for weeks or months if left untreated. The hormonal roller‑coaster after birth—plummeting estrogen and progesterone, shifting cortisol, and disrupted sleep—can throw the brain’s mood‑regulating chemistry out of whack. In particular, the GABA system, which normally keeps anxiety in check, may become under‑active, leaving you feeling jittery, tearful, or hopeless.
Red flags that merit professional attention include:
- Persistent sadness that lasts longer than two weeks
- Intense anxiety or panic attacks
- Thoughts of harming yourself or your baby
- Inability to bond with your newborn
If any of these ring true, please reach out right away. You’re not alone, and help is just a phone call away—SAMHSA’s free, confidential helpline is available 24/7.
Medical Remedies
When symptoms are moderate to severe, medication is often the fastest way to lift the fog. Below is a quick‑look at the most common prescription options, their mechanisms, and what you should watch out for.
| Remedy | How It Works | Typical Dose / Duration | Benefits | Risks / Contra‑indications |
|---|---|---|---|---|
| Standard Antidepressants (SSRIs, SNRIs) | Boost serotonin and/or norepinephrine levels | 4–6 weeks to notice effect; daily oral dose | Strong evidence, FDA‑approved for PPD | Possible sexual side‑effects, weight change; some pass into breast milk (consult your doctor) |
| Neurosteroid Drugs (e.g., brexanolone, zuranolone) | Modulate GABA‑A receptors for rapid mood lift | Brexanolone: 60‑hour IV infusion; Zuranolone: oral 14‑day course | Fastest relief reported (often within 48 h) | High cost, need for medical monitoring, limited availability; not recommended while breastfeeding |
| Adjunctive Antipsychotics (e.g., aripiprazole) | Balance dopamine & serotonin pathways | Added when monotherapy fails; daily | Helpful for severe or treatment‑resistant cases | Metabolic side‑effects, sedation |
| Hormone‑Based Treatments (estrogen/progesterone patches) | Restore postpartum hormone balance | Short‑term, under specialist supervision | May improve mood & sleep simultaneously | Risk of blood clots; not first‑line |
When you read about “antidepressants for depression,” it’s easy to think they’re all the same. In reality, each medication class has its own profile, and a psychiatrist will help match the right one to your unique situation.
Natural Options
Medical treatment doesn’t have to be a solo act. Many mothers find that adding gentle, evidence‑backed natural remedies speeds recovery and eases side‑effects. Below are the categories that consistently show up in research and real‑world success stories.
Supplements That Support Mood
Omega‑3 fatty acids (EPA/DHA) – A 2011 study from the University of Connecticut found that women who took 200 mg of DHA daily from week 24 of pregnancy through delivery scored six points lower on a postpartum depression scale than those who didn’t (study). Omega‑3s help build cell membranes in the brain, supporting serotonin and dopamine production.
Vitamin D, Magnesium, Zinc – Deficiencies are common after birth because of changing nutritional needs and lower sun exposure. Low vitamin D is linked to mood swings; magnesium can calm the nervous system; zinc supports immune health and may reduce anxiety.
Adaptogens – Herbs like ashwagandha and holy basil (Tulsi) help regulate the HPA axis, lowering cortisol and stabilizing mood without compromising breastfeeding safety.
Herbal Allies (Use With Caution)
Herbs can be a gentle boost, but always check with your OB‑GYN or pediatrician, especially if you’re nursing.
- St. John’s Wort – A potent botanical antidepressant, though it can interact with SSRIs and isn’t recommended for all breastfeeding mothers (level 2‑3 safety).
- Lemon Balm – A calming tea that lifts mood and is generally safe for lactation.
- Holy Basil (Tulsi) – Supports mental clarity and immune health; great for a mid‑day pick‑me‑up.
- Mimosa tenuiflora – Emerging research suggests it may help emotional balance, though evidence is still early.
Movement & Mind‑Body Practices
Exercise isn’t just about losing weight; it actually rewires brain chemistry. A 2023 meta‑analysis highlighted that regular aerobic activity (30 minutes, three times a week) reduces PPD severity by up to 30 %.
Try:
- Gentle walking with your stroller
- Postnatal yoga (focus on breath and core stability)
- Mindfulness‑Based Cognitive Therapy (MBCT) – combines CBT with meditation for lasting mood benefits
Sleep Hygiene
Sleep deprivation fuels the depressive loop. Simple changes can make a big difference:
- Nap when the baby naps (even 20‑minute power naps help)
- Keep the bedroom dark at night; use a soft night‑light for feedings
- If needed, discuss melatonin with your doctor—low doses are often safe while breastfeeding.
Social & Environmental Support
Loneliness is a hidden driver of PPD. Building a network doesn’t have to feel forced:
- Join a virtual “new‑mom” group on platforms like Postpartum Support International.
- Ask a trusted friend or family member to watch the baby for an hour so you can recharge.
- Consider a professional therapist who specializes in perinatal mental health.
All of these natural strategies are discussed in more depth on our postnatal depression treatment guide.
Choosing Treatment
Deciding what to try first feels overwhelming, so here’s a simple decision tree you can follow:
- Assess severity. Mild (baby blues, occasional tearfulness) → start with lifestyle tweaks: sleep, nutrition, light exercise.
- Moderate symptoms (persistent low mood, anxiety, trouble bonding) → schedule an appointment with your OB‑GYN or a psychiatrist. Discuss medication options (SSRIs, possibly neurosteroid drugs) and ask about supplement safety.
- Severe symptoms (hopelessness, intrusive thoughts, inability to care for yourself) → seek immediate care—call 911 or go to the nearest emergency department. Rapid‑acting treatments like brexanolone can be life‑changing.
Remember, it’s perfectly okay to combine approaches. Many mothers feel best when they take a prescribed SSRI, add omega‑3, walk daily, and lean on a supportive friend.
Real Stories
Let me share a quick anecdote from a friend of mine, Maya. After giving birth to twins, she felt like a “zombie” for weeks—crying at the slightest noise, unable to focus on feeding. Her doctor started her on sertraline (an SSRI) and recommended 1,000 mg of DHA daily. Within three weeks, the medication steadied her mood, but she still felt “foggy.” Maya added a 20‑minute stroller walk each afternoon and a cup of Tulsi tea after lunch. By month two, she described the “fog” as lifting, and she could finally enjoy playing with her babies. Maya’s story illustrates that even when medication does the heavy lifting, the everyday habits you add can fine‑tune the recovery.
Trusted Resources
Feeling stuck? These resources are free, confidential, and staffed by professionals who understand postpartum mental health:
- SAMHSA National Helpline: 1‑800‑662‑HELP (24/7, English & Spanish).
- Postpartum Support International: Online chat and local support groups.
- Your health‑care team: Bring a symptom journal (what you feel, when, sleep patterns) to your appointment—it speeds up diagnosis.
Quick Cheat Sheet
- Fastest medical fix: Neurosteroid infusion (brexanolone) or a well‑chosen SSRI.
- Best natural combo: Omega‑3 + Ashwagandha + 30 min daily walk.
- When to call emergency: Thoughts of harming yourself or your baby, severe insomnia, or sudden loss of appetite.
- Safety tip for breastfeeding: Check drug level ratings; most SSRIs and omega‑3 are considered safe, but always double‑check with your pediatrician.
Conclusion
Postpartum depression can feel like standing in a storm with no shelter, but the truth is there are many sturdy roofs to run under. Prescription options such as SSRIs and cutting‑edge neurosteroid drugs provide rapid relief for many, while natural allies—omega‑3s, adaptogenic herbs, gentle exercise, and a supportive community—help you rebuild steadier, longer‑lasting peace.
Take a moment right now: write down one small thing you could change this week—maybe a 10‑minute walk after dinner or a cup of lemon‑balm tea before bed. Small steps add up, and you don’t have to walk them alone.
If you have questions about any of the remedies mentioned, or simply want to share what’s worked for you, feel free to reach out. Remember, you deserve help, you deserve hope, and you deserve to feel like yourself again.





















Leave a Reply
You must be logged in to post a comment.