Hey there, friend. If you’re reading this, chances are you or someone you love is navigating the sometimes‑stormy seas of menopause and has noticed a new, uneasy relationship with food. Maybe you’ve started obsessively counting calories, feel a sudden urge to binge, or you’re scared of the dreaded “menopause weight gain.” You’re not alone, and this isn’t just “in your head.” Hormonal shifts, body‑image worries, and life‑stage stress can all combine to spark menopause eating disorders. In the next few minutes we’ll unpack why that happens, how to spot the signs, and—most importantly—what you can actually do about it, all in a chatty, no‑judgment voice.
Why Hormones Matter
First up: the science, but don’t worry—no PhD required. During the menopausal transition estrogen and progesterone dip dramatically. Those hormones are like the conductors of a symphony that includes your brain’s reward system, appetite signals, and mood regulation. When they waver, the “music” can get out of sync, leading to cravings, mood swings, and a feeling that food suddenly controls you.
- Estrogen decline reduces serotonin, the “feel‑good” neurotransmitter, which can make you seek out high‑sugar foods for a quick mood boost. (according to Healthline)
- Progesterone fluctuations affect the brain’s reward pathways, making binge‑eating feel oddly rewarding.
- Sleep disturbances—night sweats, hot flashes, insomnia—mess with ghrelin and leptin, hormones that tell you when you’re hungry or full.
All of that adds up to a perfect storm for disordered eating menopause patterns, whether it’s the sneaky “just one cookie” habit that spirals or a sudden drive to restrict everything.
Spotting Red Flags
When your mind starts to revolve around food, weight, or body image more than it used to, it’s time to listen. Below is a quick “self‑check” you can run through. Tick any that feel familiar:
| Eating‑Disorder Symptom | Menopause‑Specific Twist |
|---|---|
| Obsessive calorie counting | Using apps obsessively after a hot‑flash episode |
| Secret binge episodes | Bingeing after a night of poor sleep |
| Extreme food restriction | Avoiding carbs because “weight gain is inevitable” |
| Purging or laxative misuse | Choosing laxatives to “reset” after a hormonal surge |
| Pre‑occupation with body image | Feeling “out of control” as abdominal fat appears |
If three or more of these resonate, consider reaching out to a professional. Early detection can prevent the cascade that leads to serious health issues like osteoporosis or heart disease.
How It Differs
Most of us think of eating disorders as a teenage problem, but the data says otherwise. A 2025 National Geographic report found that women in their 40s‑60s are twice as likely to have an eating disorder as they are to develop breast cancer. The type of disorder also shifts with the menopausal stage:
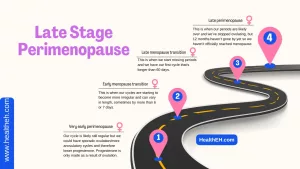
- Perimenopause (the years leading up to your last period) often brings binge‑eating spikes.
- Post‑menopause (after 12 months without a period) tends to see more restrictive or “clean‑eating” obsessions.
Why? During perimenopause, hormone swings are most erratic, feeding binge urges. Once the ovaries quiet down, the body craves control, and that can manifest as severe restriction or orthorexia—obsessive “healthy” eating that can become just as harmful.
Treatment Options
Good news: there are evidence‑based pathways that actually work. Below is a toolbox you can start pulling from right now.
Professional Therapy
Cognitive‑Behavioral Therapy for Eating Disorders (CBT‑EDI) is the gold standard recommended by NICE. It helps you untangle thoughts (“I’m gaining weight, so I must stop eating”) from behaviours (binge‑eating, restriction). Interpersonal Psychotherapy (IPT) targets the life‑stage stressors that often trigger the disorder—think empty nest, caring for aging parents, career shifts.
Medical Interventions
Hormone‑replacement therapy (HRT) can smooth the estrogen roller‑coaster, reducing cravings and mood swings. A 2024 review in Maturitas highlighted that women on HRT reported fewer binge episodes compared to those not using it. Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine are also helpful for binge control.
Nutrition Guidance
Balance isn’t about “diet” in the restrictive sense—it’s about menopause diet tips that keep you full, nourished, and satisfied:
- Prioritise protein at each meal (helps preserve muscle mass).
- Include fiber‑rich foods (vegetables, legumes) to steady blood sugar.
- Healthy fats (avocado, nuts, olive oil) support hormone production.
- Avoid crash diets; they only amplify the urge to binge later.
Working with a registered dietitian who knows the menopausal landscape can personalize these tips and keep you from falling into “all‑or‑nothing” thinking.
Lifestyle & Self‑Care
- Mind‑body practices—yoga, meditation, or even a 10‑minute breathing exercise—lower cortisol, the stress hormone that fuels cravings.
- Sleep hygiene—keep the bedroom dark, limit caffeine after 2 p.m., and establish a calming bedtime routine to curb night‑time hunger.
- Movement you enjoy—not a treadmill marathon, but a brisk walk, dancing in the kitchen, or a gentle swim.
Support Networks
Isolation only deepens the problem. Communities like the Balance Menopause forum provide peer‑to‑peer support where you can share victories and setbacks without judgment. If you ever feel unsafe or think about self‑harm, call NHS 111 or your local crisis line immediately.
Real Stories
Stories make the data feel human. Here are three women who walked the same path and found their way out.
Kirstie, 42 – The Relapse
Kirstie, a commercial lawyer, had battled anorexia in her teens. When perimenopause hit, the sudden changes in her body reminded her of the control she once sought through restriction. “It was like my old voice whispered, ‘You can’t let this happen again,’” she told The Independent. With a therapist specializing in mid‑life eating disorders and a gentle HRT regimen, she learned to replace restriction with mindful nourishment.
Julie, 51 – The Calorie‑Counting Spiral
Julie’s story was featured in Women’s Health. After a routine menopause check‑up, the fear of “menopause weight gain” drove her to count every calorie. Within months she was glued to a scale and felt panic whenever the treadmill broke. A free assessment at Priory’s Life Works Hospital helped her see that the numbers were not her identity. Today she focuses on balanced meals and regular movement rather than perfect numbers.
Anna, 57 – Finding Community
Anna, a retired teacher, discovered binge‑eating after her mother’s diagnosis of osteoporosis. She felt “out of control” and turned to food for comfort. Joining an online support group at Balance Menopause gave her a safe space to talk, and a dietitian helped her create a meal plan that honored her cravings while stabilizing blood sugar. She now reports fewer binge episodes and a stronger sense of self‑worth.
First‑Step Toolkit
Ready to take action? Here’s a simple, no‑pressure checklist you can start today.
- Self‑screen – Grab a piece of paper and answer the symptom table above.
- Journal – For two weeks note mood, hot flashes, and any eating episodes. Patterns will emerge.
- Schedule a check‑in – Call your GP or a menopause‑specialist. Bring your notes.
- Try one diet tip – Add a protein‑rich snack (Greek yogurt, handful of nuts) after any hot flash to curb cravings.
- Connect – Sign up for a peer‑support forum (like Balance Menopause) and share your first step.
These tiny steps might feel modest, but they create a roadmap out of the fog.
Quick Recap
Menopause can bring a hidden companion: menopause eating disorders. Hormonal turbulence, shifting body image, and life‑stage stressors can turn food into a coping tool, leading to bingeing, restriction, or other disordered patterns. The good news is that early detection, professional therapy, possible hormone treatment, tailored nutrition, and supportive communities can restore balance.
Remember, you’re not “just getting older” and then suddenly “acting weird.” Your brain and body are reacting to real physiological changes, and seeking help is a sign of strength, not weakness. If any part of this resonated with you, take a breath, pick one item from the First‑Step Toolkit, and give yourself permission to ask for support. You deserve compassion, clarity, and the chance to thrive—menopause and all.
What’s your experience with food and menopause? Have you found a tip that helped? Drop a comment, share your story, or simply let us know you’re not alone. We’re in this together.























Leave a Reply
You must be logged in to post a comment.