If you’ve started getting “surprise” periods that seem to arrive at random, you’re probably wondering what on earth is happening to your body. The quickest way to make sense of the chaos is to begin perimenopause period tracking. A few minutes each day can reveal when menopause is looming, which symptoms belong to which phase, and when it’s time to call your doctor. Below we’ll walk through simple paper templates, the best free apps, and what the data can tell you about hormones, mood, and sleep. By the end you’ll have a ready‑to‑use tracker, a checklist of red‑flags, and practical tips to turn raw numbers into real‑world relief.
Why tracking matters
Tracking isn’t just about noting dates; it’s about gaining insight, control, and confidence. Here are the biggest wins (and a couple of caution points) you’ll get from a consistent perimenopause period tracker.
| Benefit | Potential risk / misconception |
|---|---|
| Spot menopause early → better treatment timing | Over‑reliance on apps may miss subtle hormonal “bleeds”. |
| Identify symptom patterns (hot flashes, mood swings) → more focused doctor visits | Privacy concerns – choose apps with strong data policies. |
| Track cycle‑length changes → gauge ovulation status | Mistaking an anovulatory bleed for a true period. |
According to Healthline, keeping a log helps you recognize when menopause is truly approaching—once you’ve gone a year without bleeding. WomenLivingBetter notes that a shortening cycle is often the first sign perimenopause has begun, so catching that early can be a game‑changer.
Getting started
What to log each day
- Start & end date of bleeding – the first‑day rule is the gold standard.
- Flow intensity – light / medium / heavy or a 1‑3 scale.
- Associated symptoms – hot flashes, mood shifts, sleep quality, cravings, headaches, etc.
- Lifestyle factors – stress level, caffeine/alcohol intake, exercise, medication changes.
- Basal body temperature (BBT) – if you’re curious about ovulation (more on that later).
Paper templates you can copy
Two printable tables work for almost anyone. Print them – or draw them in a notebook – and fill them out each day.
| Date | Day # | Cycle Length | Flow (1‑3) | Notes (symptoms, meds) |
|---|---|---|---|---|
| [Copy the row for each day] | ||||
For a more granular view, try the daily log below. It’s perfect if you’re also tracking BBT or cervical fluid.
| Date | BBT (°C) | Cervical Fluid | Mood (1‑5) | Sleep hrs | Pain/Discomfort | Notes |
|---|---|---|---|---|---|---|
| [Copy the row for each day] | ||||||
You can download these PDFs from CeMCOR – they’re free and ready to print.
Choosing a digital app
If you prefer your phone to do the heavy lifting, here’s a quick side‑by‑side look at the most popular options.
| App | Free tier? | Perimenopause‑specific features | Privacy note |
|---|---|---|---|
| Balance app | Yes | Hormone‑phase alerts, symptom journal, menopause‑focused articles | Data stored locally; export available. |
| Flo | Yes | Cycle‑length trends, custom symptom tags, community support | Uses anonymized aggregation; optional cloud backup. |
| Clue | Paid after trial | Advanced BBT & temperature graphs, hormonal phase predictions | GDPR‑compliant, encrypted storage. |
| Any calendar | Free | Simple event entry, color‑code flows | No health‑data sharing. |
Each of these apps lets you export a CSV file, making it easy to switch tools later without losing data.
Understanding the numbers
Cycle length & menopause timeline
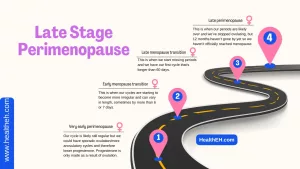
The average perimenopausal transition lasts about four years, according to Healthline. A rule of thumb: once you’ve gone 12 months without any bleeding (including spotting), you’ve officially entered menopause.
Basal body temperature (BBT) and anovulatory cycles
BBT is your body’s resting temperature first thing in the morning, before you even swing your legs out of bed. After ovulation, progesterone causes a tiny but measurable spike (usually ~0.3 °C) that stays high until your next period. If that rise never shows up, it’s a sign you didn’t ovulate—a common scenario in perimenopause.
Here’s a quick cheat‑sheet to read your temperature chart:
| Pattern | Likely scenario |
|---|---|
| Sustained > 0.3 °C rise mid‑cycle | Ovulation confirmed |
| No rise, flat line | Anovulatory cycle → low progesterone |
| Drop after day 18‑20 | Hormonal bleed, not a true period |
Marie Kesteen’s 2024 guide (source) emphasizes that tracking BBT can tell you whether a bleed is a genuine period or just a progesterone‑driven “spotting” episode—information that can prevent unnecessary hormone therapy.
Linking symptoms to hormonal phases
- Early follicular phase (low estrogen) – hot flashes, low energy, occasional cravings.
- Luteal phase (low progesterone) – mood swings, insomnia, breast tenderness, bloating.
- Anovulatory cycles – irregular spotting, heightened anxiety, shorter cycles.
When you start seeing these patterns on paper (or screen), you’ll be able to ask your clinician very specific questions, rather than vague “I feel off” statements.
Real‑world stories
Anna, 48, irregular cycles
Anna started using a simple notebook template after noticing a sudden five‑day delay between periods. Three months later she saw her cycle length shrink from 29 days to 22 days—a classic sign that perimenopause had kicked in. She showed the chart to her OB‑GYN, who confirmed the hormonal shift and started a low‑dose progesterone regimen. Within six weeks Anna reported fewer night sweats and steadier moods.
Sofia, 52, on a fertility app
Sofia loved the visual graphs of her “fertility” app, but after four consecutive cycles showed no BBT rise, the app warned her: “No ovulation detected.” She switched to a combined approach—BBT plus cervical‑fluid tracking (the “egg‑white” consistency). The new data revealed occasional anovulatory bleeds that had masqueraded as light periods. With this clarity, she avoided an unnecessary hormone‑replacement prescription and instead focused on lifestyle tweaks (diet, sleep hygiene).
These anecdotes illustrate how a few minutes of logging can save time, money, and emotional stress. If you have a story of your own, we’d love to hear it in the comments!
Choosing the right tracker
Paper vs. app vs. hybrid
| Format | Cost | Privacy | Ease of use | Flexibility |
|---|---|---|---|---|
| Paper notebook | $0‑$5 | Highest (offline) | Simple, tactile | Limited analytics |
| Mobile app | Free‑$30/yr | Variable (check policy) | Immediate alerts | Rich charts, export |
| Hybrid (paper + spreadsheet) | Minimal | High (local files) | Slight learning curve | Custom formulas, graphs |
Switching without losing data
If you decide to move from a paper diary to an app, export your notebook pages as a CSV (you can scan them with Microsoft Lens) and import into the new platform. Most apps let you import a CSV, preserving dates, flow levels, and notes. Likewise, when you jump from one app to another, simply use the built‑in “export data” function and re‑import.
Quick‑start checklist
- Pick your tracking method (paper, app, or both).
- Download or draw a template – use the PDFs linked above.
- Record today’s date, flow level, and any symptom you notice.
- Set a nightly reminder for BBT (if you’re measuring).
- Review your log every Sunday – look for trends, not isolated days.
Commit to 30 days and you’ll already have a mini‑report to discuss with your healthcare provider.
Expert & resource recommendations
For deeper dives, consider these trustworthy sources:
- Dr. Jerilynn C. Prior’s research on estrogen “storm” patterns – CeCMOR provides a free daily diary to capture those fluctuations.
- American College of Obstetricians & Gynecologists (ACOG) clinical guidelines on managing perimenopause symptoms.
- Peer‑reviewed studies on BBT accuracy (2023) – useful if you’re leaning on temperature data.
- Healthline’s practical step‑by‑step guide (linked above) for choosing apps and interpreting trends.
Whenever you cite an external source, make sure the link opens in a new tab and respects user privacy – that’s why we add rel="nofollow noreferrer" and target="_blank" attributes.
Final thoughts
Starting to track now—even with a plain notebook—gives you a roadmap through the hormonal roller‑coaster of perimenopause. Choose a tool that feels comfortable, stay consistent, and use the patterns you spot to have informed conversations with your clinician. The result? Early detection of menopause, smarter symptom management, and a stronger sense of control over your body.
Ready to begin? Download the free printable tracker, set a 30‑day logging challenge, and share the biggest insight you discover in the comments below. Let’s demystify perimenopause together, one day at a time.





















Leave a Reply
You must be logged in to post a comment.